Although the technology is relatively new, there is a growing body of research that demonstrates the efficacy of confocal laser endomicroscopy (CLE), illustrating its broad application and future potential.
By Auriane Olivier, Mauna Kea Technologies
A timely, accurate diagnosis can be life-changing for millions of people who are diagnosed with complex or chronic lung disease. And it has become increasingly clear that as the occurrence of these conditions continues to grow, clinicians need technology that will allow them to quickly and accurately deliver a diagnosis and evaluate the condition, monitor the progression of the disease, and inform personalized treatment over time.
Even prior to the COVID-19 pandemic, the incidence of life-threatening lung disease was consistently on the rise, year after year. These conditions are difficult to diagnose, contribute significantly to healthcare costs, and diminish quality of life for patients. To understand the need for technology that improves the diagnosis and monitoring of lung disease, simply consider the fact that an estimated 236,740 new cases of lung cancer will be diagnosed in the United States in 2022, and 1-in-16 people will get lung cancer in their lifetime. Meanwhile, although it may not be the media story of the day, lung cancer remains the leading cause of cancer deaths among men and women in the United States.
Statistics about chronic lung disease are equally troubling. More than 16 million people in the United States have COPD, which is also a primary cause of death. There are more than 200 forms of interstitial lung disease (ILD), and 55% of people with ILD receive at least one misdiagnosis, while 38% receive two or more misdiagnoses prior to an accurate diagnosis. Given the rate of occurrence for these conditions, it’s not surprising that the cost of care for the 37 million Americans who are living with chronic lung disease is also substantial, with US workers paying $7 billion for asthma treatment from 2011-2015 and $5 billion for treatment of COPD.
The Power of Sight
Visibility into cellular changes within lung tissue and in lung nodules is crucial to accurately pinpointing, assessing, and diagnosing changes in lung physiology. For example, 80% of lung lesions are at the periphery of the lung, which means traditional bronchoscopic procedures may not effectively locate potentially dangerous nodules. Meanwhile, poor or limited access to the tissue in question can lead to inaccurate biopsy results and can impede the ability to monitor and treat nodules.
To successfully manage the future of lung health and improve treatment and outcomes for patients with lung cancer, COVID strains, and other respiratory conditions, interventional pulmonologists and thoracic specialists need the ability to access a lung nodule through tissue targeting, see inside that nodule, and evaluate the potential disease state.
How in vivo Cellular Imaging Can Help

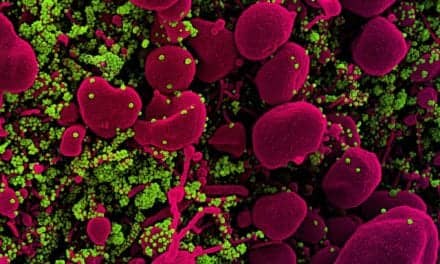
Because the most deadly and life changing lung diseases often present few, if any, early symptoms, access to real-time, in vivo, cellular activity allows physicians to accurately and more quickly diagnose and monitor lung health, and to evaluate a patient’s reaction to therapies as they occur within the body.
Confocal laser endomicroscopy (CLE) is a technology with many applications in pulmonology and lung health. Two proven CLE applications are needle-based confocal laser endomicroscopy (nCLE), which is used with manual and robotic-assisted bronchoscopy procedures in the treatment of lung nodules, and probe-based confocal laser endomicroscopy (pCLE), which is used in the treatment and management of ILD, COPD, and related diseases.
In my work with clinicians who use Cellvizio, for example, real-time in vivo cellular imaging delivers visibility of cellular activity that enables physicians to evaluate areas of concern in cases where conventional disease screening returns ambiguous results, and allows physicians to characterize areas of interest or concern with confidence1. In the future, nCLE could make it possible for physicians to monitor point-in-time reactions as they happen within the body during drug delivery, so they can observe and understand cause and effect responses and determine the optimal course of action for each patient. Meanwhile, nCLE allows clinicians to plan, intervene and treat patients more precisely during image-guided procedures. These capabilities combine to directly support the growth of personalized, precision medicine for lung disease.

nCLE also integrates with robotic-assisted procedures by enhancing a physician’s ability to confirm needle placement and optimize diagnostic yield. This could lead to less invasive, more precise diagnostic procedures and targeted surgical treatments. Clinical studies are underway to provide further evidence validating the use of nCLE with robotic-assisted procedures.
Although the technology is relatively new, there is a growing body of research that demonstrates the efficacy of nCLE, illustrating its broad application and future potential. For example, published research shows that nCLE is effective in the diagnosis of peripheral lung nodules; and more specifically, that bronchoscopic nCLE imaging in peripheral lung cancer is feasible, safe, and allows real-time malignancy detection at the tip of the needle with an accuracy equal to 95%, demonstrating the potential of nCLE imaging as a real-time guidance tool to reduce the bronchoscopic near-miss rate.1 In addition, the accuracy of nCLE imaging for detecting malignancy in tumors and metastatic lymph nodes was 90% and 89% respectively.2
Lung cancer is just one area where CLE technology has produced positive results. The technology also has applications in managing the progression of ILD and long COVID, where pCLE has the capability to accurately assess the density of alveolar thickened fibers, the disorganization of elastin network, and multiple large drops of intra alveolar secretions in patients with COVID.3 Research has also shown that pCLE can differentiate between mild and dense fibrotic lung tissue and distinguish between the pleura and the alveolar airspaces, which accordingly, could diminish the complication rate for patients with ILD.3

Lung health has never been more of a priority for our world than it is right now, but the need for technology that enables clinicians to deliver personalized, precision medicine extends beyond lung cancer, COPD, ILD, and long COVID to existing and evolving diseases. Fortunately, with CLE technology like Cellvizio, physicians have the potential to change the course of treatment, outcomes, and quality of life for patients with a wide variety of conditions that compromise lung health.
Auriane Olivier is senior US Account Manager for Mauna Kea Technologies, a global medical device company that manufactures and sells Cellvizio, the real-time in vivo cellular imaging platform. For more information contact [email protected].
References
- Kramer T, et al. Bronchoscopic needle-based confocal laser endomicroscopy (nCLE) as a real-time detection tool for peripheral lung cancer. Thorax. 25 June 2021. doi: 10.1136/thoraxjnl-2021-216885
- Wijmans L, et al. Needle-based confocal laser endomicroscopy for real-time diagnosing and staging of lung cancer. ERJ. 2019 53: 1801520; https://doi.org/10.1183/13993003.01520-2018
- Wijmans L, et al. Confocal laser endomicroscopy as a guidance tool for transbronchial lung cryobiopsies in interstitial lung disorder. Respiration. 2019;97:259-263. doi: 10.1159/000493271