Having a bacterial infection in the blood, known as bacteremia, at the same time as COVID-19 is a greater risk factor for COVID-19 death, intensive care unit admission, and mechanical ventilation than previously described risk factors such as advanced age, male sex, or various comorbidities, according to a retrospective cohort study led by the University of Alabama at Birmingham researchers.
The study, published in the journal Critical Care, reviewed 13,781 COVID-19 inpatient encounters from 2020 to 2022 at UAB Hospital and Ochsner Louisiana State University Health Shreveport hospitals and divided them into three groups: confirmed bacterial co-infection, as measured by a blood test at 48 hours after admission; suspected bacterial co-infection in patients receiving antimicrobials; and no bacterial co-infection.
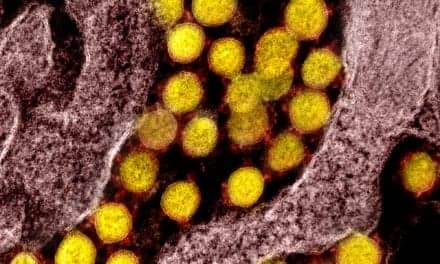
Bacterial co-infection is a known major source of sickness and death in the context of other respiratory viral infections such as influenza, parainfluenza, or respiratory syncytial virus. However, it has been unclear regarding the frequency of bacteremic co-infection in COVID-19 and the impact it has on clinical outcomes.
“Although confirmed bacteremic co-infections are rare in COVID-19, less than 4% of inpatient admissions, our results show that COVID-19 patients with these co-infections have a staggering 25% risk of death at 30 days in UAB patients and a similar risk of 20% at Ochsner Louisiana State University Health Shreveport, or OLHS,” says Amit Gaggar, MD, PhD, UAB Department of Medicine Division of Pulmonary, Allergy, and Critical Care Medicine, in a press release.
Gaggar, in collaboration with the Hugh Kaul Precision Medicine Institute director Matthew Might, PhD, and infectious disease physician-scientist Nathaniel Erdmann, MD, PhD, co-led the study.
“These results strongly suggest an underappreciated interaction between bacterial pathogens and the COVID-19 virus, SARS-CoV-2, and their impact on clinical outcomes,” says Erdmann in a press release.
Specifically, researchers found that the in-hospital mortality for COVID-19 co-infections of 26% at UAB and 22% at OLHS exceeded that of the suspected co-infection (UAB, 24%; OLHS, 12%) and the no co-infection groups (UAB, 5.9%; OLHS, 5.1%). Furthermore, a control group of 1,703 UAB inpatients with community-acquired bacteremias during a period before the COVID-19 pandemic had a 5.9% in-hospital mortality rate.
The researchers also identified laboratory trends associated with COVID-19 bacterial co-infection—a neutrophil-to-lymphocyte ratio of 15 or greater and the systemic inflammatory response syndrome criteria of abnormal white blood cell counts or a heart rate greater than 90 beats per minute. These can help health care providers discriminate COVID-19 bacterial co-infections within 24 hours of admission.
“These results emphasize the role of bacteria in SARS-CoV-2 mortality and highlight the potential for neutrophil-to-lymphocyte ratio as a rapid and easily available prognostic biomarker of bacterial coinfection and, relatedly, disease severity,” says Might in a press release.
Strengths of the study were the two large, demographically diverse, independent cohorts—UAB reflects an academic hospital and Level I trauma center serving five surrounding states, and OLHS includes encounters from rural, suburban, and academic medical centers across Louisiana. Both cohorts overall were well matched for patient age, race, sex, and inpatient length of stay.