Using high-frequency chest wall oscillation for COPD and bronchiectasis patients resulted in reduced antibiotic use, emergency room or urgent care visits, and hospitalizations.
By Beth Foley and Harley Metcalfe, RRT
Aim
Analyze the potential benefit of adding AffloVest therapy to patients with COPD/bronchiectasis.
Background
Chronic obstructive pulmonary disease (COPD) is a disease of the lungs that causes obstructed airflow that results in breathing problems.¹ Bronchiectasis is a chronic lung disease that causes the airways to narrow due to inflammation, reducing the ability of the cilia to effectively carry mucus up and out of the lungs. This causes the patient to have a difficult time expectorating mucus, which in turn puts the patient at higher risk for infection in the lungs, as well as having to deal with a chronic cough.² Studies show that 42% of patients with COPD will also have bronchiectasis.³
Currently, COPD is the third leading cause of death in the US.¹ Along with the increased risk of death, COPD has a detrimental effect on the patient’s quality of life. Patients experience not only a chronic cough, but also lack of energy and a disrupted sleep pattern. Frequent exacerbations requiring multiple antibiotic therapy, ER visits and hospitalizations are common. A study by Elflein in November 2020’s Statista showed that 85% of patients with COPD have had at least one exacerbation in the last year.⁴
Airway clearance therapy is a cornerstone therapy for the prevention and treatment of pulmonary disease. Early diagnosis and implementation of airway clearance can reduce morbidity and mortality.⁵ One form of airway clearance therapy is high-frequency chest wall oscillation (HFCWO). The goal of HFCWO is to loosen, thin and mobilize a patient’s lung secretions for easier removal. HFCWO has been shown to reduce hospitalization rates for COPD patients without bronchiectasis. A recent study in CHEST showed that HFCWO provided an overall reduction of 54% in annualized hospitalization rates for respiratory causes and a 20% reduction in patients with three or more hospitalizations.⁶
Introduction
For this study, 30 patient charts were reviewed to compare the need for antibiotic therapy due to exacerbation, based on number of prescriptions, ER/Urgent care visits and hospitalizations in the period before each patient started HFCWO therapy compared to the period after initiating HFCWO therapy.
Patient Demographics
The average age of the patient population was 74 years old, with 14 male participants and 16 female participants. All patients were prescribed AffloVest HFCWO therapy twice per day for 30 minutes each session.
Methods
- Randomly selected 30 patients, from internal patient database, utilizing AffloVest HFCWO therapy
- Patient group sorted, by year, according to initiation of AffloVest therapy:
- 10 (2017)
- 7 (2018)
- 13 (2019)
- All patients followed-up, via phone, to verify therapy was being utilized as prescribed; baseline was 23.3 months post therapy
- Reviewed pre- and post- chart notes, using a double-blind review of all data
- Reviewers compared findings; discrepancies resolved by mutual review of chart
- Recorded specific patient data on excel spreadsheet for final review
- Calculated patient response and average of post therapy symptom outcome
- Finalized compliance and outcome study
Outcomes
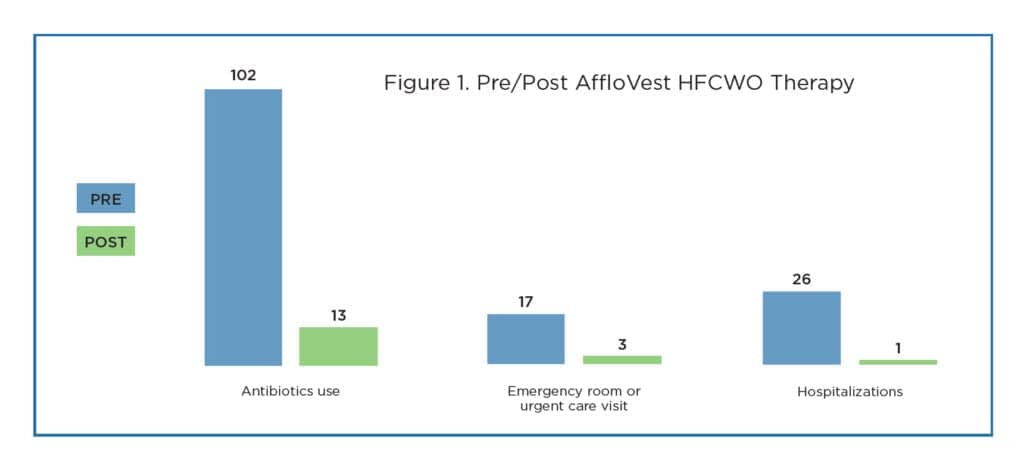
Patients using AffloVest HFCWO therapy had a reduction in the need for ER/Urgent care visits, hospitalizations, and antibiotics to treat exacerbations.
The comparison was made with chart notes before therapy with AffloVest began and the period after initiating therapy with AffloVest. The cumulative range of qualifying chart notes (Pre) was 175.3 months with an average amount of time per patient of 5.8 months. The cumulative range of post-therapy notes (Post) was 186 months with an average amount of time per patient of 6.2 months. The post therapy comparison included both chart notes and self-reporting follow up phone calls made by Advanced Medical DME staff to the patient directly. Any discrepancy between the chart notes and follow up phone call was resolved by secondary chart note review.
After initiating AffloVest therapy a dramatic reduction was observed in antibiotic use, ER/Urgent care visits and hospitalizations. There were 26 hospitalizations before initiating therapy, compared to just one after therapy began, a 96.2% reduction. There were 17 ER/Urgent Care visits before initiating therapy, with only three after therapy began, an 82.4% reduction.
Regarding antibiotics usage, there were 102 prescriptions for antibiotics pre-therapy, and only 13 post-therapy, an 87.3% reduction. Antibiotic resistance is a growing threat to global health. The overuse of antibiotics and the trend to minimize their use due to antibiotic-resistant infections is something to consider. A growing number of infections, like pneumonia and tuberculosis, are becoming harder to treat and more costly as antibiotic resistance leads to less effective medicines, longer hospital stays and higher medical costs.⁷
Patients also reported symptom relief when using the AffloVest HFCWO therapy. Besides exacerbations, symptoms such as shortness of breath, lack of energy and poor quality of sleep affect patients with COPD over time and depending on severity of disease.
Advanced Medical DME had an extensive follow-up care program. Patients and/or caregivers were called after initiating AffloVest therapy at the following intervals: seven days, 30 days, 60 days, and every 180 days thereafter. Patients were asked a series of questions, as listed in Figure 2. Patients then answered numerically, based on the key (listed in Figure 2).
Of the 30 patients in this study, Advanced DME was able to contact 14. Figure 2 represents the cumulative average of the 14 patients surveyed within the follow-up period. The questions were subjective based on the patient’s condition that day, or the caregiver’s understanding of the patient’s symptomatic history. The results showed that patients overall felt that their AffloVest therapy improved their symptoms.
Conclusion
A team approach to follow up care by the DME provider, patient, and clinic staff is vital for continued symptom improvement, quality of life and healthcare savings. Early implementation of airway clearance therapy has been shown to reduce morbidity and mortality and HFCWO therapy has been shown to benefit COPD patients. In this study, reduced antibiotic use, ER/urgent care visits and hospitalizations in 30 patients using AffloVest HFCWO therapy were observed.
Beth Foley, BS, and Harley Metcalfe, BS, RRT, are employed by Advanced Medical DME, a multistate respiratory-focused provider with 15 years of experience in home medical equipment. For more information, contact [email protected].
Editor’s note: This study was conducted by Advanced Medical DME and submitted by International Biophysics Corporation. IBC funded the study.
References
- Elflein J. COPD in the U.S. – Statistics and Facts. August 2019. www.statista.com/topics/4339/chronic-obstructive-pulmonary-disease
- COPD Foundation. Bronchiectasis and COVID. October 2020. www.copdfoundation.org/COPD360social/community/COPD-Digest/Article/1610
- Kosmas E, et al. Bronchiectasis in Patients with COPD: An Irrelevant Imagery Finding of Clinical Important Phenotype? CHEST 2016; 150(4):894A.
- Elflein J. Exacerbation in the Past Year among those with COPD in the U.S. as of 2020. www.statista.com/statistics/921791/copd-past-year-exacerbation-us/us
- Volsko T. Airway Clearance Therapy: Finding the Evidence, Respiratory Care 2013; 58(10):1669-78.
- Barto T, et al. Outcomes of High Frequency Chest Wall Oscillation (HFCWO) in COPD Patients without Bronchiectasis. CHEST 2019; 156(4): Supplement A1170.
- World Health Organization. Antibiotic Resistance Facts. July 2020. https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance