Clinical trial and real-world data provide evidence that inhaled nitric oxide is effective for reducing perioperative pulmonary hypertension.
By iJayne Prats, PhD; iiDavid E. Stocker, PharmD; and iiiCharles V. Pollack Jr, MA, MD
Abstract
Observational data indicate that nitric oxide (NO) gas has been widely used in pediatric and adult cardiac surgery in the US for over a decade, whether administered by inhalation/ventilation or directly into the cardiopulmonary bypass circuit. This perioperative use of iNO in cardiac surgery is consistent with labeled indications in other, ex-US jurisdictions, and has become standard practice in many large centers in the US. Such use, however, while approved in several regulatory jurisdictions worldwide, remains off-label in the US.
In this review, the mechanism of action for NO and its clinical relevance to cardiac surgery is presented, including preoperative, intraoperative, and postoperative periods (collectively, “perioperative”). This review includes observational data from US practice over the past decade. These data consistently show that the use of NO in cardiac surgery is common and has in fact become a practice standard at many institutions. Although the use of inhaled NO (iNO) in the US remains off-label, reviews by the European Medicines Agency (EMA), Australian, Japanese, and various Latin American health agencies [need references/websites] have granted a label indication for inhaled NO based on these data, which were interpreted as supportive of patient safety and have important and consistent efficacy signals.
Mechanism of Action of Inhaled Nitric Oxide and Clinical Relevance
Inhaled nitric oxide (iNO) is a potent selective dilator of pulmonary vessels and therefore can directly reduce pulmonary vascular resistance (PVR). Thus, iNO therapy as a selective pulmonary vasodilator in cardiac surgery, with the specific goal of lowering pulmonary pressure, represents a significant pharmacological advance in managing perioperative pulmonary hemodynamics and life-threatening right ventricular dysfunction (RVD) and failure in this setting.
The mechanism of action of inhaled NO is well understood; after inhalation into the alveolus, NO produces smooth muscle relaxation by increasing intracellular levels of cyclic guanosine monophosphate (cGMP) within the pulmonary vascular smooth muscle.1 This leads to the activation of cGMP-dependent kinases (cGKs), which in turn leads to the activation of myosin phosphate and a subsequent release of calcium from intracellular stores, thereby allowing smooth muscle cells to relax.
As the NO further diffuses into the vessel lumen, it is bound to and inactivated by oxyhemoglobin. The bound hemoglobin is converted to methemoglobin and further reduced to nitrates and nitrites. Therefore, the vasodilatory effects of NO are localized to the pulmonary vasculature and are short lived, because the half-life of cGMP is less than one minute.2
Pulmonary Hypertension in Cardiac Surgery
Pulmonary hypertension with RVD is one of the most common complications encountered intra- and post-operatively in both pediatric3 and adult4 cardiac surgery patients, and can complicate the treatment course for the cardiac surgery patient despite maximum pharmacologic and ventilatory support.1,5,6 Cardiac surgical patients may develop RVD for various reasons during the perioperative period.4
In the absence of PH or left ventricular dysfunction (LVD), this change may not cause important hemodynamic compromise. In the setting of elevated RV afterload or coexisting left ventricular dysfunction (LVD), however, the RV may be unable to generate the required stroke volume to achieve adequate pulmonary flow. Diminished pulmonary flow subsequently leads to a lower preload and decreased cardiac output. The hemodynamic implications of RVD depend not only on the degree of myocardial contractile dysfunction, but also on the loading conditions imposed on the RV. Pulmonary vascular resistance is the primary determinant of RV afterload, and therefore reducing PVR may improve RV performance.
Several factors peculiar to cardiopulmonary bypass (CPB) may also contribute to elevations in PVR during cardiac surgery. Cardiopulmonary bypass produces endothelial injury; when this occurs in the pulmonary vasculature, a transient elevation in PVR commonly results. Secondly, as a result of hemolysis that is caused by passage of blood through the CPB pump in cardiac surgery, hemoglobin is released into the circulation in the form of oxyhemoglobin. Endogenous NO binds to oxyhemoglobin, and NO depletion by plasma oxyhemoglobin promotes pulmonary vasoconstriction and impairs tissue perfusion. Other contributing factors include impaired endogenous NO production, increased release of endothelin, the inflammatory response to CPB, and the release of vasoactive substances, such as thromboxane, microemboli, leucosequestrati on, and hypoxic pulmonary vasoconstriction, which results from alveolar edema and atelectasis.7
Whether or not CPB is required, however, PH is an important prognostic factor in cardiac surgery. In clinical trials PH is associated with. and is an accepted surrogate endpoint for increased morbidity and mortality.4 With an aging population and the associated increased severity of illness, the prevalence of PH in cardiac surgical patients will increase.
Acute Kidney Injury in Cardiac Surgery
Another consideration in the aging population is the development of acute kidney injury (AKI) in association with CPB for cardiac surgery. Outside the pulmonary circulation, depletion of NO by free oxyhemoglobin in the kidneys facilitates development of AKI by intrarenal oxidative reactions.8 Acute kidney injury after cardiac surgery is common, with some reports citing a figure close to 30%, although the exact incidence varies with definition and based on the numerous scoring systems available.9 About 1%–2% of patients develop severe renal injury requiring dialysis, and AKI after cardiac surgery is associated with a substantial increase in morbidity and mortality.9 Even when there is only a modest increase in serum creatinine values from baseline values, AKI is associated with longer hospital stay and increased costs.9
The administration of exogenous NO gas oxidizes plasma oxyhemoglobin to methemoglobin and might thus prevent cardiac surgery-associated AKI.10 Supportive data have been published both for inhaled NO and for addition of NO into the cardiopulmonary bypass pump oxygenator.9,11
The pathophysiology of AKI after cardiac surgery is complex and multifactorial.12 Likely mechanisms of injury include microembolization, neurohormonal activation, exogenous and endogenous toxins, metabolic as well as hemodynamic and inflammation factors, ischemia-reperfusion injury, and oxidative stress. The consequence of these insults, which are likely interrelated and synergistic, is a cascade of reflex changes within the kidney leading to a common presentation of AKI manifesting as impairment of renal function, persistent renal vasoconstriction, an exaggerated response to exogenous vasoconstrictors, and vascular endothelial and tubular epithelial cell death due to necrosis and apoptosis.13
Regional blood flow and renal vasomotor tone are particularly altered by the use of CPB, which activates systemic inflammatory response, generates microemboli, and alters vasomotor tone (reducing renal parenchymal oxygen tension, and consequently, decreasing the renal perfusion pressure up to 30%), thereby increases the ischemia–reperfusion injury.14 Studies have indicated that NO is protective against ischemia-reperfusion injury in kidney transplant procedures.15-16
The release of free hemoglobin secondary to hemolysis is associated with renal tubular damage as well as increased systemic vascular resistance, platelets and coagulation activity dysfunction, and increased mortality.17 Nitric oxide scavenges free hemoglobin and reduces the impact of this mechanism of injury.
Inhaled Nitric Oxide Use in Cardiac Surgery
Pulmonary hypertension and elevated PVR in all clinical settings are usually responsive to iNO.18
The vasodilatory effects of NO are localized to the pulmonary vasculature and are short lived, because the half-life of cGMP is less than one minute.2 This allows the near immediate cessation of the effects of NO when it is removed from the respiratory circuit. This moment-to-moment, highly localized effect is potentially both safe and efficacious in the critical care management of the cardiac surgical patient. On the other hand, the use of intravenous vasodilators may improve RV function,4 but the systemic hypotension associated with the use of these agents may further impair myocardial perfusion and ventricular function, especially in the perioperative environment.
Most of our understanding of the use of iNO in cardiac surgery comes from consistent data derived from small observational or single center randomized trials. Nonetheless, perioperative iNO has been approved for use in both children and adults in multiple regulatory jurisdictions, while in the US, off-label use of iNO in this setting is often the most frequent use of iNO in hospitals with cardiac surgery capability. Therefore, perioperative iNO represents a “practice standard” in cardiac surgery even though iNO use is off-label in this setting and cannot from the clinical trial literature be considered a “gold standard.”
Summary of Clinical Trial Data
The published clinical trial literature on the use of iNO in the perioperative management of patients undergoing cardiac surgery and experiencing PH or acute right ventricular decompensation reflects a concordance of clinically meaningful results indicating safety and efficacy.
While the literature is neither particularly broad nor deep, with only a few well-designed, rigorously executed, adequately powered studies with consistent dosing and duration of treatment, and while there is an absence of a statistically significant mortality effect attributable to iNO, there are consistent findings of:
- Reduction in pulmonary artery pressure and PVR among patients with acute PH in the perioperative environment;
- Selective effect on pulmonary hemodynamics as evidence by the lack of systemic hypotension as an adverse event (AE) in these trials;
- Similar efficacy in infants (10-20 ppm), children (10-20 ppm), and adults (20 40 ppm);
- General trends towards improvement in important clinical and pharmacoeconomic outcomes such as time to weaning off cardiac bypass, RV function support, intubation time (and success of extubation), and length of ICU stay are seen with NO perioperatively;
- Lower incidence of post-operative acute kidney injury (AKI) associated with cardiopulmonary bypass;
- Pervasive safety, as indicated by a general absence of consistent or persistent adverse effects in this setting, including clinically significant methemoglobinemia;
- Lack of a comparator found to be more effective or safer.
There are also additional biologically plausible signals that perioperative iNO in patients undergoing cardiac surgery and experiencing PH or acute RV decompensation experience
- Lower incidence of intra- and post-operative myocardial injury;
- Improvement in intra- and post-operative cardiac index;
- Fewer perioperative pulmonary hypertension “crises.”
Importantly, no large Phase 3 trial of iNO in the perioperative cardiac surgery space has been performed. There are two clear reasons for this:
- iNO is known to be effective in treating PH in all age groups, and therefore it would be unethical to perform a placebo-controlled trial.
- There is no universally accepted alternative gold standard therapy, and therefore, a comparator-controlled trial of iNO is not feasible. The current practice standard use of iNO means that enrollment in such a large trial would prove difficult to recruit.
Several categories of clinical trials are summarized in the following tables that have supported label expansion into perioperative cardiac surgery use in the ex-US jurisdictions, plus the few trials completed since the latest ex-US approval (Australian TGA for adults, in April 2019). A search for relevant studies was performed in PubMed using the terms “inhaled nitric oxide” and “cardiac surgery,” limited to humans, and clinical trials. The search returned 168 results, which were reviewed for relevance, and included in Tables 1-3 for adult cardiac surgery, adult transplant surgery and ventricular assist device placement, and pediatric cardiac surgery.
Adult Cardiac Surgery
The published adult, nontransplant surgery clinical trial experience comprises 361 patients in 9 trials.19-29 (See Table 1.) Comparators to NO studied in this setting included IV nitroglycerin, IV milrinone, IV nitroprusside, IV PGE1, inhaled prostacyclin, and placebo. Dosing of NO ranged from 10 to 40 ppm, but duration and start time (on pump, in recovery) varied. No study showed a mortality benefit attributed to iNO use, but several of the secondary efficacy endpoints were positive. As expected, iNO had a salutary effect on pulmonary hemodynamics. Among these are reductions in the incidence and severity of AKI in association with cardiac surgery requiring CPB in patients who received iNO treatment.8,11 The safety profile of iNO was favorable across these studies.
Adult Transplant, LVAD
Cardiac Transplantation. Pulmonary hypertension in the cardiac transplant recipient is a major cause of right-side heart failure and early death. Goals in the management of acute RV failure include preservation of coronary perfusion through maintenance of systemic blood pressure and reducing RV afterload by decreasing the PVR.6 Inhaled NO has been shown to selectively reduce PVR and to enhance RV stroke work after cardiac transplantation.30
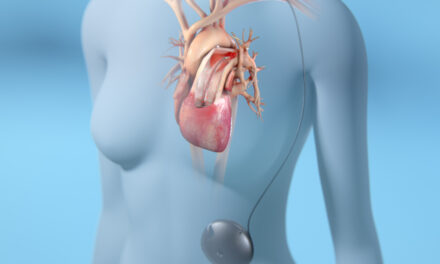
Insertion of Left Ventricular Assist Device (LVAD). Right ventricular dysfunction occurs in 20% to 50% of patients after insertion of an LVAD.31 The ability of the RV to pump enough blood to the LVAD is critically related to the intrinsic contractility of the RV and the RV afterload, which is influenced by the PVR. The PVR is usually elevated in patients with long-standing congestive heart failure and can be further increased in the early postoperative period by the effects of CPB. A trial of iNO is recommended before implantation of an RV assist device is considered because this invasive procedure may be avoided if there is a salutary response to iNO.32 In a randomized, double-blinded trial, Argenziano and coworkers) demonstrated the hemodynamic benefits of iNO (decreased pulmonary artery pressure and increased LVAD flow) in LVAD recipients with pulmonary hypertension.33
The published adult, transplant surgery/LVAD implantation clinical trial experience comprises 301 patients in 7 trials.34-40 (See Table 2.) Comparators to iNO studied in this setting included IV nitroprusside, IV PGE1, inhaled prostacyclin, and placebo. Doses of iNO ranged from 20 to 40 ppm, but duration and start time (pre-op, intra-op, post-op) varied. No study showed a mortality benefit associated with iNO use, but several of the secondary efficacy endpoints as listed above were positive. When pulmonary hemodynamics were measured, iNO had a beneficial effect on these parameters, as expected. The safety profile of iNO was favorable across these studies.
Pediatric Surgery
The published pediatric, non-transplant surgery published clinical trial experience comprises 315 patients in eight trials.41-48 (See Table 3). Comparators to iNO studied in this setting included IV milrinone, inhaled prostacyclin, sildenafil, hyperventilation, “conventional therapy,” and placebo. Doses of iNO ranged from 20 to 30 ppm, but duration and start time (on pump, on separation from pump) varied. No study showed a mortality benefit associated with iNO use, but several of the secondary efficacy endpoints were positive. When pulmonary hemodynamics were measured, as expected iNO had a beneficial effect on these parameters. The safety profile of iNO was favorable across these studies; in particular, methemoglobin levels in these patients remained below 2%, with one exception (transient excursion to 8%) and in another study, the maximum methemoglobin was 3.4%.
Use of INO in Real World Registries, Observational Studies, and Meta-Analyses
Inhaled Nitric Oxide Treatment of Perioperative Pulmonary Hypertension
In the perioperative setting, iNO at 10-30 ppm is used to support oxygenation in patients undergoing surgeries up to and including heart transplant, lung transplant, and implantation of LVADs.49 In cardiac applications, including transplants, PH can lead to right-sided heart failure and early death. Inhaled NO can reduce right ventricular stroke work while not reducing systemic blood pressure. In lung transplantation, iNO is administered in an effort to attenuate ischemia-reperfusion injury, which is an early cause of transplant rejection. Similarly, after LVAD placement, iNO-driven reductions in RV afterload can result in increased left ventricular (LV) filling, LVAD flow, and overall cardiac output.
Reduction in the Incidence of AKI Associated with CPB in Cardiac Surgery
Because administration of NO gas in models was observed to lower plasma NO consumption in the presence of hemolysis, studies have been conducted to assess the potential for NO to decrease the risk of AKI associated with CPB.
Lei et al8 randomized 244 patients undergoing elective, multiple valve replacement surgery (mostly due to rheumatic fever) to receive either 80 ppm iNO (treatment) or nitrogen (control). The purpose of the study was to determine whether NO reduced the incidence of postoperative AKI and improved long-term kidney outcomes after multiple cardiac valve replacement requiring prolonged (more than 90 minutes) CPB. Nitric oxide and nitrogen were administered at the same dose, via the gas exchanger (oxygenator) during CPB, and by inhalation for 24 hours postoperatively. The primary outcome was oxidation of ferrous plasma oxyhemoglobin to ferric methemoglobin, indicating scavenging of free hemoglobin. Secondary outcomes were AKI transition to Stage 3 chronic kidney disease (CKD) at 90 days and one year, and major adverse kidney events.
The primary outcome was associated with reduced postoperative AKI from 64% (control) to 50% (NO group). Transition to Stage 3 CKD at 90 days was reduced from 33% (control) to 21% (NO) and at one year, from 31% to 18%. Nitric oxide treatment reduced the overall major adverse kidney events at 30 days, 90 days, and one year. These outcomes were numerically, but not significantly, lower for NO treatment: index hospitalization RRT was required in 3% of the patients in the NO group versus 5% in the control group, and mortality rates at 1 year were 3% and 6%, respectively. The authors concluded that in patients undergoing multiple valve replacement and prolonged CPB, administration of NO decreased the incidence of AKI, transition to Stage 3 chronic kidney disease, and major adverse kidney events at 30 days, 90 days, and one year.
A second randomized controlled study was conducted in 96 patients with moderate preoperative risk of renal complications who underwent cardiac surgery with CPB. Kamenshchikov et al randomized patients to either NO supplementation (40 ppm) in the CPB bypass circuit during the entire CPB period (NO group; n=48) or usual care (control group; n=48).11 Unlike the Lei study, iNO was not administered post-operatively. The primary outcome of this trial was the 48 hour incidence of AKI.
NO administration was associated with a significant decrease in total AKI incidence: 10 (20.8%) in NO group versus 20 (41.6%) in the control group. Two cases of Stage 2 AKI were observed in the NO group (4.1%), versus five cases (10.4%) in the control group. One case of Stage 3 AKI requiring RRT occurred in the control group. Secondary outcomes such as urinary output (a predictor of renal complications) were significantly higher in the NO group; urinary neutrophil gelatinase-associated lipocalin (uNGAL) levels at four hours after surgery were significantly lower in the NO group compared with the control group. Elevated uNGAL levels are predictive for worse long-term outcomes of cardiac surgery, AKI onset, prolonged hospital stay, need for RRT, and mortality. The uNGAL level during the postoperative period is itself of clinically significant. Authors concluded that NO administration in patients at moderate risk of renal complications undergoing elective cardiac surgery with CPB was associated with a lower incidence of AKI.
Hu et al50 conducted a systematic review and meta-analysis to determine the effect of NO gas on renal function and other clinical outcomes in patients requiring CPB. The primary outcome was the RR of AKI, irrespective of the AKI Stage. The secondary outcome was the mean difference (MD) in the length of ICU and hospital stay, the RR of postoperative hemorrhage, and the MD in levels of methemoglobin. Of 54 studies assessed, five studies (579 patients) were eligible for meta-analysis. In the studies, NO was administered at doses of 10, 40, or 80 ppm. The Lei and Kamenshchikov studies discussed above were included.
NO was associated with reduced risk of AKI. In a subgroup analysis by NO initiation timing, NO did not decrease the risk of AKI when started at the end of CPB. However, NO did significantly reduce the risk of AKI when started from the beginning of CPB. In this meta-analysis, NO did not affect the length of ICU and hospital stay or the risk of postoperative hemorrhage. NO slightly increased the level of methemoglobin at the end of CPB, but the increase was deemed to be clinically negligible. The authors concluded that overall NO appeared to reduce the risk of postoperative AKI in patients undergoing CPB. Indeed, the accumulated data that demonstrates reduction in the incidence of AKI during CPB with NO may be sufficient to support a separate indication.
Treatment of Patients Undergoing Surgical Treatment of Congenital Heart Disease
Postoperative pulmonary hypertensive crises are an important cause of morbidity and mortality after surgery for congenital heart disease.5 and may be precipitated by diminished NO production resulting from endothelial dysfunction.51 Inhaled NO has been reported to ameliorate the postoperative PH of congenital heart disease52 and to decrease the need for postoperative ECMO.53 In a randomized double-blind study, Miller and colleagues examined the effects of the prophylactic use of iNO in high-risk infants undergoing congenital heart surgery.54 They reported that compared with placebo, infants who after surgery inhaled 10 ppm NO continuously until just before extubation had fewer pulmonary hypertensive crises and shorter times to eligibility for extubation.
Inhaled Nitric Oxide Use in Pediatric Cardiac Surgery
In the 20 years since the initial limited approval for NO in neonates, there has been no regulatory action to expand the label for patients beyond term/near term neonates with PPHN. However, physicians at US children’s hospitals have been increasingly using NO for off-label diagnoses. Available information suggests that this trend applies to most Children’s Hospital Association (CHA)-member hospitals that participate in regularly sharing their performance data.
The Children’s Hospital Association surveyed its member hospitals in 2016 to determine trends in utilization of NO. The surveyed hospitals reported >15% off-label use, with 12 of the 22 hospitals reporting some use of NO finding an increase in NO use over 2013.55
A presentation at the 2018 Society of Critical Care Medicine meeting reported on observational data from 43 hospitals in the Pediatric Health Information Systems between 2005 and 2015, for pediatric patients receiving iNO during hospitalization.56 In total, 18,343 patients (median age at admission was 28 days old (IQR=0–324 days) qualified for inclusion. There were 836 patients in 2005 and 1,986 patients in 2015. Overall mortality was 22.7%. Mortality was 29.1% in 2005 and 21.2% in 2015.
The APR-DRG classes associated with the highest number of admissions with NO use included: “tracheostomy with mechanical ventilation more than 96 hours with extensive procedure or extracorporeal membranous oxygenation (ECMO)” (n=1909), “major cardiothoracic repair of heart anomaly” (n=1722), followed by “neonate birth weight >2,499 grams with major cardiovascular procedure” (n=1324). The non-surgical class associated with the highest number of admissions with iNO use was “respiratory diagnosis with ventilation 96+ hours” (n=1013).
This large observational analysis for the use of iNO in pediatric patients indicates a trend towards increased use over the 10-year study period. There was a concomitant trend toward a decrease in mortality over the 10-year study period. Most of the NO was used in patients requiring ECMO and cardiac surgery.
Real-World Nitric Oxide Utilization
Nitric oxide for inhalation was approved by the FDA in the US in 1999, with the single indication to improve oxygenation and reduce the need for ECMO in term and near-term (>34 weeks gestation) neonates with hypoxic respiratory failure (HRF) associated with clinical or echocardiographic evidence of pulmonary hypertension, termed “PPHN” for persistent pulmonary hypertension in the newborn, in the hospital setting.
With NO widely available in many US hospitals, there have been notable increases in use outside the neonatal intensive care unit, particularly in the cardiac catheterization laboratory and in the perioperative management of patients undergoing major cardiothoracic surgery and orthotopic organ transplant surgery.
LEK Consulting LLC conducted an evaluation of the NO market place in 2017. They estimated that approximately 50,000 patients were treated with NO each year in US hospitals. Twelve percent of the use of NO was on-label; 82% of the use was outside of labelling, with 39% of that use associated with adult/pediatric cardiac surgery.57
Global Regulatory Landscape
Perioperative iNO has been approved for use in both children and adults in multiple regulatory jurisdictions, namely the EU, Australia, Japan, and several Latin American countries. In the US, the off-label use of inhaled NO in this setting is often the most frequent use in hospitals with cardiac surgery capability.
Table 4 reflects the global regulatory landscape for cardiovascular surgery. The list is accurate as of June 2021.
The indicated dosing for pediatric cardiac surgery patients is an initial 10 ppm, up to 20 ppm if needed. Adults in this setting are dosed at an initial 10-20 ppm up to 40 ppm. The lowest effective dose should be used. As in any indication, patients should be monitored PaO2, methemoglobin and NO2.
Summary
Although the only US FDA-approved indication for iNO has remained for use in neonatal patients with persistent pulmonary hypertension, several other worldwide regulatory jurisdictions have approved iNO for perioperative use in adults and pediatric patients undergoing cardiac surgery. As outlined in this review, clinical trial and real-world data provide evidence that iNO is effective for reducing pulmonary hypertension in the perioperative setting. The use of iNO is widespread, and its use has become the practice standard for surgical teams.
RT
This manuscript was supported and submitted by Vero Biotech Inc. For more information, contact [email protected].
Author Affiliations
i. Jayne Prats, PhD, (literature search, manuscript preparation) works for Elysis LLC (Carlisle, MA) and is a consultant to Vero Biotech.
ii. David E. Stocker, PharmD, (manuscript review) is chief operating officer of Vero Biotech (Atlanta, GA).
iii. Charles V. Pollack Jr, MA, MD, (manuscript preparation) is vice president Medical Communications and Scientific Affairs, Vero Biotech (Atlanta, GA).
References
- Ichinose F, Roberts JD Jr, Zapol WM. Inhaled nitric oxide: a selective pulmonary vasodilator: current uses and therapeutic potential. Circulation. 2004;109:3106-11.
- Van Haastert PJ, Van der Heijden PR. Excitation, adaptation, and deadaptation of the cAMP-mediated cGMP response in Dictyostelium discoideum. J Cell Biol. 1983;96:347-53.
- Lindberg L, Olsson AK, Jögi P, Jonmarker C. How common is severe pulmonary hypertension after pediatric cardiac surgery? J Thorac Cardiovasc Surg. 2002;123:1155-63.
- Denault A, Deschamps A, Tardif JC, Lambert J, Perrault L. Pulmonary hypertension in cardiac surgery. Curr Cardiol Rev. 2010;6:1-14.
- Hopkins RA, Bull C, Haworth SG, et al. Pulmonary hypertensive crises following surgery for congenital heart defects in young children. Eur J Cardiothorac Surg. 1991;5:628–34.
- Stobierska-Dzierzek B, Awad H, Michler RE. The evolving management of acute right-sided heart failure in cardiac transplant recipients. J Am Coll Cardiol. 2001;38:923–31.
- Wessel DL, Adatia I, Giglia TM, Thompson JE, Kulik TJ. Use of inhaled nitric oxide and acetylcholine in the evaluation of pulmonary hypertension and endothelial function after cardiopulmonary bypass. Circulation. 1993;88(5 Pt 1):2128-38.
- Lei C, Berra L, Rezoagli E, Yu B, Dong H, Yu S, et al. Nitric Oxide Decreases Acute Kidney Injury and Stage 3 Chronic Kidney Disease after Cardiac Surgery. Am J Respir Crit Care Med. 2018;198:1279-87.
- Mahaldar AR, Sampathkumar K, Raghuram AR, et al. Risk prediction of acute kidney injury in cardiac surgery and prevention using aminophylline. Indian J Nephrol. 2012;22:179-83.
- Gangadharan S, Sundaram KR, Vasudevan S, et al. Predictors of acute kidney injury in patients undergoing adult cardiac surgery. Ann Card Anaesth. 2018;21:448-54.
- Kamenshchikov NO, Anfinogenova YJ, Kozlov BN, et al. Nitric oxide delivery during cardiopulmonary bypass reduces acute kidney injury: A randomized trial. J Thorac Cardiovasc Surg. 2020:S0022-5223(20)31541-5.
- Bellomo R, Auriemma S, Fabbri A, et al. The pathophysiology of cardiac surgery-associated acute kidney injury (CSA-AKI). Int J Artif Organs. 2008;31:166-78.
- Vives M, Hernandez A, Parramon F, et al. Acute kidney injury after cardiac surgery: prevalence, impact and management challenges. Int J Nephrol Renovasc Dis. 2019;12:153-66.
- Okusa MD. The inflammatory cascade in acute ischemic renal failure. Nephron. 2002;90:133-8.
- Phillips L, Toledo AH, Lopez-Neblina F, Anaya-Prado R, Toledo-Pereyra LH. Nitric oxide mechanism of protection in ischemia and reperfusion injury. J Invest Surg. 2009;22:46-55.
- Meade MO, Granton JT, Matte-Martyn A, et al, Toronto Lung Transplant Program. A randomized trial of inhaled nitric oxide to prevent ischemia-reperfusion injury after lung transplantation. Am J Respir Crit Care Med. 2003;167: 1483–9.
- Vercaemst L. Hemolysis in cardiac surgery patients undergoing cardiopulmonary bypass: a review in search of a treatment algorithm. J Extra Corpor Technol. 2008;4:257-67.
- Chester AH, Yacoub MH, Moncada S. Nitric oxide and pulmonary arterial hypertension. Glob Cardiol Sci Pract. 2017;Jun 30(2):14.
- Schmid R, Bürki C, Engel MHC, et al. Inhaled Nitric Oxide Versus Intravenous Vasodilators in Severe Pulmonary Hypertension After Cardiac Surgery. Anesth Analg:1999;89:1108-15.
- Solina A, Papp D, Ginsberg S, et al. A comparison of inhaled nitric oxide and milrinone for the treatment of pulmonary hypertension in adult cardiac surgery patients. J Cardiothorac Vasc Anesth. 2000;14:12-7.
- Solina AR, Ginsberg SH, Papp D, et al. Dose response to nitric oxide in adult cardiac surgery patients. J Clin Anesth. 2001;13:281-6.
- Gianetti J, Del Sarto P, Bevilacqua S, et al. Supplemental nitric oxide and its effect on myocardial injury and function in patients undergoing cardiac surgery with extracorporeal circulation. J Thorac Cardiovasc Surg. 2004;127(1):44-50.
- Fattouch K, Sbraga F, Bianco G, et al. Inhaled prostacyclin, nitric oxide, and nitroprusside in pulmonary hypertension after mitral valve replacement. J Card Surg. 2005;20(2):171-6.
- Fattouch K, Sbraga F, Sampognaro R, et al. Treatment of pulmonary hypertension in patients undergoing cardiac surgery with cardiopulmonary bypass: a randomized, prospective, double-blind study. J Cardiovasc Med (Hagerstown). 2006;7:119-23.
- Winterhalter M, Simon A, Fischer S, et al. Comparison of inhaled iloprost and nitric oxide in patients with pulmonary hypertension during weaning from cardiopulmonary bypass in cardiac surgery: a prospective randomized trial. J Cardiothorac Vasc Anesth. 2008;22:406-13.
- Fernandes JL, Sampaio RO, Brandão CM, et al. Comparison of inhaled nitric oxide versus oxygen on hemodynamics in patients with mitral stenosis and severe pulmonary hypertension after mitral valve surgery. Am J Cardiol. 2012;107:1040-5.
- Matamis D, Pampori S, Papathanasiou A, et al. Inhaled NO and sildenafil combination in cardiac surgery patients with out-of-proportion pulmonary hypertension: acute effects on postoperative gas exchange and hemodynamics. Circ Heart Fail. 2012;5:47-53.
- Lei C, Berra L, Rezoagli E, et al. Nitric Oxide Decreases Acute Kidney Injury and Stage 3 Chronic Kidney Disease after Cardiac Surgery. Am J Respir Crit Care Med. 201;198:1279-87.
- Kamenshchikov NO, Anfinogenova YJ, Kozlov BN, et al. Nitric oxide delivery during cardiopulmonary bypass reduces acute kidney injury: A randomized trial. J Thorac Cardiovasc Surg. 2020:S0022-5223(20)31541-5.
- Ardehali A, Hughes K, Sadeghi A, et al. Inhaled nitric oxide for pulmonary hypertension after heart transplantation. Transplantation. 2001;72: 638–41.
- Frazier OH, Rose EA, Macmanus Q, et al. Multicenter clinical evaluation of the HeartMate 1000 IP left ventricular assist device. Ann Thorac Surg. 1992;53:1080–90.
- Yahagi N, Kumon K, Nakatani T, et al. Inhaled nitric oxide for the management of acute right ventricular failure in patients with a left ventricular assist system. Artif Organs. 1995;19:557–8.
- Argenziano M, Choudhri AF, Moazami N, et al. Randomized, double-blind trial of inhaled nitric oxide in LVAD recipients with pulmonary hypertension. Ann Thorac Surg. 1998;65:340–5.
- Kieler-Jensen N, Ricksten SE, Stenqvist O, et al. Inhaled nitric oxide in the evaluation of heart transplant candidates with elevated pulmonary vascular resistance. J Heart Lung Transplant. 1994;13:366-75.
- Argenziano M, Choudhri AF, Moazami N, et al. Randomized, double-blind trial of inhaled nitric oxide in LVAD recipients with pulmonary hypertension. Ann Thorac Surg. 1998;65:340-5.
- Rajek A, Pernerstorfer T, Kastner J, et al. Inhaled nitric oxide reduces pulmonary vascular resistance more than prostaglandin E(1) during heart transplantation. Anesth Analg. 2000;90:523-30.
- Ardehali A, Hughes K, Sadeghi A, et al. Inhaled nitric oxide for pulmonary hypertension after heart transplantation. Transplant 2001;72:638-41.
- Radovancevic B, Vrtovec B, Thomas CD, et al. Nitric oxide versus prostaglandin E1 for reduction of pulmonary hypertension in heart transplant candidates. J Heart Lung Transplant. 2005;24:690-5.
- Potapov E, Meyer D, Swaminathan M, et al. Inhaled nitric oxide after left ventricular assist device implantation: a prospective, randomized, double-blind, multicenter, placebo-controlled trial. J Heart Lung Transplant. 2011;30:870-8.
- Khan TA, Schnickel G, Ross D, et al. A prospective, randomized, crossover pilot study of inhaled nitric oxide versus inhaled prostacyclin in heart transplant and lung transplant recipients. J Thorac Cardiovasc Surg. 2009;138:1417-24.
- Goldman AP, Delius RE, Deanfield JE, Macrae DJ. Nitric oxide is superior to prostacyclin for pulmonary hypertension after cardiac operations. Ann Thorac Surg. 1995;60:300-5.
- Russell IA, Zwass MS, Fineman JR, et al. The effects of inhaled nitric oxide on postoperative pulmonary hypertension in infants and children undergoing surgical repair of congenital heart disease. Anesth Analg. 1998;87:46-51.
- Day RW, Hawkins JA, McGough EC, Crezeé KL, Orsmond GS. Randomized controlled study of inhaled nitric oxide after operation for congenital heart disease. Ann Thorac Surg. 2000;69:1907-12.
- Miller OI, Tang SF, Keech A, Pigott NB, Beller E, Celermajer DS. Inhaled nitric oxide and prevention of pulmonary hypertension after congenital heart surgery: a randomised double-blind study. Lancet. 2000;356:1464-9.
- Morris K, Beghetti M, Petros A, Adatia I, Bohn D. Comparison of hyperventilation and inhaled nitric oxide for pulmonary hypertension after repair of congenital heart disease. Crit Care Med. 2000;28:2974-8.
- Stocker C, Penny DJ, Brizard CP, Cochrane AD, Soto R, Shekerdemian LS. Intravenous sildenafil and inhaled nitric oxide: a randomised trial in infants after cardiac surgery. Intensive Care Med. 2003;29:1996-2003.
- Khazin V, Kaufman Y, Zabeeda D, et al. Milrinone and nitric oxide: combined effect on pulmonary artery pressures after cardiopulmonary bypass in children. J Cardiothorac Vasc Anesth. 2004;18:156-9.
- Cai J, Su Z, Shi Z, et al. Nitric oxide in conjunction with milrinone better stabilized pulmonary hemodynamics after Fontan procedure. Artif Organs. 2008;32:864-9.
- Oz MC, Ardehali A. Collective review: perioperative uses of inhaled nitric oxide in adults. Heart Surg Forum. 2004;7:E584-9.
- Hu J, Spina S, Zadek F, et al. Effect of nitric oxide on postoperative acute kidney injury in patients who underwent cardiopulmonary bypass: a systematic review and meta-analysis with trial sequential analysis. Ann Intens Care. 2019;9:129.
- Celermajer DS, Cullen S, Deanfield JE. Impairment of endothelium-dependent pulmonary artery relaxation in children with congenital heart disease and abnormal pulmonary hemodynamics. Circulation. 1993;87:440–6.
- Roberts JD Jr, Lang P, Bigatello LM, Vlahakes GJ, Zapol WM. Inhaled nitric oxide in congenital heart disease. Circulation. 1993;87:447–53.
- Goldman AP, Delius RE, Deanfield JE, et al. Pharmacological control of pulmonary blood flow with inhaled nitric oxide after the fenestrated Fontan operation. Circulation. 1996; 94 (suppl II): II44–II48.
- Miller OI, Tang SF, Keech A, Pigott NB, Beller E, Celermajer DSl. Inhaled nitric oxide and prevention of pulmonary hypertension after congenital heart surgery: a randomised double-blind study. Lancet. 2000;356:1464–9.
- Children’s Hospital Association presentation on CHA Utilization of Nitric Oxide, 2016, personal communication.
- Chan J. Evaluating Ten Years of Inhaled Nitric Oxide Use In Pediatric Patients. Critical Care Med. 2018;46 (suppl):236
- Vero Biotech, Data on File.