In pregnant women, SARS-CoV-2 fetal inflammation can occur even if the virus does not infect the placenta, according to a study by the National Institutes of Health.
Researchers describe unique maternal, fetal, and placental immune responses among pregnant women with COVID-19 in a study led by NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). The findings detail changes in antibodies, immune cell types and inflammatory markers in maternal blood, umbilical cord blood and placental tissues.
According to the CDC, people who are pregnant are at a higher risk for severe illness from COVID-19, compared to people who are not pregnant. COVID-19 during pregnancy also increases the risk for preterm birth, stillbirth and preeclampsia. Therefore, understanding COVID-19 infection during pregnancy is important to help healthcare providers optimize the health and safety of their patients during the pandemic.
The study, published in Nature Communications, evaluated 23 pregnant women. Twelve were positive for SARS-CoV-2, and of these, eight were asymptomatic, one had mild symptoms and three had severe COVID-19. After delivery, the researchers compared immune responses between mothers and their newborns by comparing maternal blood and umbilical cord blood. Inflammatory immune responses triggered by the virus were observed in women, their neonates and placental tissues regardless of whether the mothers had symptoms.
The study team described the following observations:
- Pregnant women with SARS-CoV-2 had a reduction in an immune cell type called T-cells, which helps drive antiviral responses.
- Mothers with SARS-CoV-2 infection developed antibodies against the virus whether or not they had symptoms, and some of these antibodies were found in the umbilical cord blood.
- Infected mothers had a higher level of immune activity markers (ie, cytokines) in blood regardless of symptoms. The elevated cytokines are interleukin-8, interleukin-15 and interleukin-10.
- Infants born to infected mothers, even if the mother had no symptoms, had an inflammatory response reflected by higher levels of interleukin-8. This elevation was observed even though the fetus presumably did not have COVID-19.
- While SARS-CoV-2 virus was absent in placentas, the placentas from infected mothers had altered ratios of immune cell types. The researchers also found altered immune activity (measured by changes in RNA transcripts) in the placenta and cord blood of infants born to infected mothers. These findings indicate that the fetal inflammation can occur during maternal infection by SARS-CoV-2 even if the virus is not detected in the placenta.
Overall, the findings will help researchers better understand COVID-19 during pregnancy, the NIH reports. The authors note that the key observation is that maternal infection with SARS-CoV-2 induces a fetal immune response even in the absence of placental infection or symptoms in the newborn. Therefore, the potential long-term effects of this inflammatory process on infants requires further study.
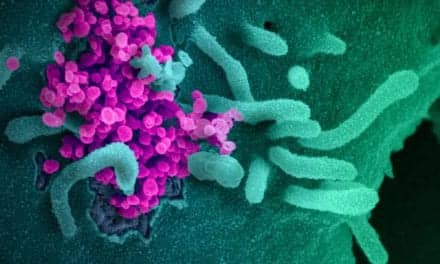
SARS-CoV-2 Fetal Inflammation