Researchers have found that adding genetic information to a former or current smoker’s clinical risk profile results in a reclassification of their risk for lung cancer in about 1-in-4 patients, according to a study presented at ATS 2015.
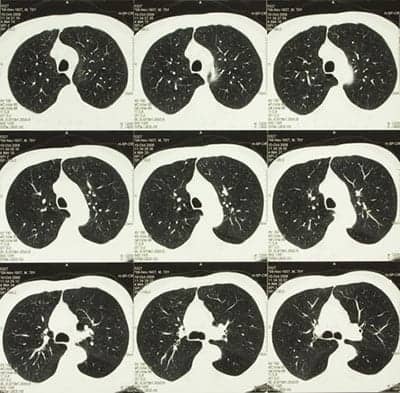
Preliminary findings from their lung cancer screening feasibility study also suggests that those whose genetic and clinical risk placed them in the highest risk category were more likely to adhere to follow-up computed tomography (CT) scans during screening.
While past studies have demonstrated that participation in lung cancer screening is improved in the context of risk assessment, this is the first study to report on the effects of gene-based risk assessment and screening adherence.
“Outside clinical trials, adherence to screening is typically 50 to 60 percent,” said lead investigator Robert Young, MD, PhD, associate professor of medicine and molecular genetics, at the University of Auckland, New Zealand, who will present the results at ATS 2015, May 15 to 20 in Denver. “What our study shows is that risk assessment using personal genetic information is not only of great interest to screening participants, it appears to improve their compliance with screening.”
The genetic component represents the net effect of 20 single nucleotide polymorphisms (SNPs) that have been implicated in the development of lung cancer by Young and other research groups. When present, these SNPs confer either an increased risk of lung cancer (12 susceptibility-related SNPs) or a reduced risk (8 protective-related SNPs). With this personal genetic information, the researchers reclassified 28% of the participants: 22% were re-assigned to a higher risk category and 6% to a lower one.
Overall adherence to the CT screening follow-up protocol was 63%. As expected, adherence was greatest in the very high risk category: 71%. Those in the high and moderate risk categories both had 52% adherence. The difference was significant (71% vs 52%, OR=2.3, P<0.05).
“Not only does adding personalized genetic data contribute to a better assessment of lung cancer risk, it appears to improve screening adherence,” Young said.