A group of scientists from the Karolinska Institutet in Sweden have discovered how the brain controls breathing in response to changing carbon dioxide and oxygen levels in the blood. A new study in mice found that the brain releases a small molecule called Prostaglandin E2 (PGE2) to help protect itself and regulate breathing when exposed to decreased oxygen or increased carbon dioxide levels. To discover the mechanism, the research team grew a section of a mouse’s brainstem in a particular type of dish.
The slice contained an arrangement of nerve and supporting cells, which allowed it to breathe for 3 weeks. During this time, the team monitored the cells and their behavior in response to changes in the environment, reports Medical Xpress.
“Our novel brainstem culture first revealed that cells responsible for breathing operate in a small-world network. Groups of these cells work very closely with each other, with each group interconnected by a few additional cells that appear to work as hubs,” explains David Forsberg, PhD, the first author of the study. “This networking activity and the rhythmic respiratory motor output it generated were preserved for the full 3 weeks, suggesting that our brainstem can be used for long-term studies of respiratory neural network activity.”
In addition, Forsberg says the team observed that exposure to different substances made the brainstem breathe faster or slower. “Perhaps most interesting was its response to carbon dioxide, which triggered a release of PGE2. Here, PGE2 acted as a signaling molecule that increased breathing activity in the carbon dioxide-sensitive brainstem region, leading to slower and deeper breaths…” says Forsberg.
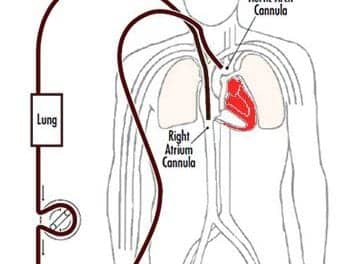
The new insights have significant implications for babies, who experience notably reduced levels of oxygen during birth. At this stage, PGE2 protects the brain and prepares the brainstem to generate deep sigh-like breath intakes, resulting in the first breaths of air following birth, according to Medical Xpress. In addition, the study also reveals a pathway linking the inflammatory and respiratory systems. PGE2 is released during inflammation and fever, which can deregulate breathing patterns and interfere with normal responses to carbon dioxide and can in turn cause disturbed or dangerous halts in breathing.
“Our findings go some way to explaining how and why our breathing responses to imbalanced oxygen and carbon dioxide levels are impaired during infectious episodes. It also helps further our understanding of why infection can inhibit breathing so severely in newborn babies,” says senior author of the paper Eric Herlenius. “We now want to find out how breaths form and develop during episodes of inflammation. This could be useful for researching potential new ways to save babies’ lives when they are unable to catch their breaths.”
Photo Credit: Neurolex
Source: Medical Xpress