Practitioners honored a family’s request to withdraw respiratory intervention. The results were not expected.

EP, a 61-year-old male, was a patient in the intensive care unit of a small, semirural hospital in Ohio. Prior to this admission, he had a 10-year history of chronic obstructive pulmonary disease and congestive heart failure. Four years ago, because of difficulty clearing secretions, he had a tracheostomy tube inserted. Since then, he had become well known to the hospital staff. The current admission was his second in the month.
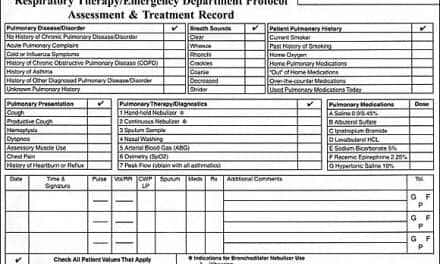
During the present admission, he preferred to keep the tracheostomy tube capped with the inner cannula removed, as was his custom at home. He was receiving oxygen via nasal cannula at four liters per minute. In addition, he received 2.5 mg albuterol mixed with 0.5 mg ipratropium via small volume nebulizer every 4 hours. Throughout the early evening, EP had been alert and oriented. He had exhibited some mild respiratory distress, especially with exertion; however, that was normal for his condition. His SpO2 on the nasal cannula was 94%. His heart rate was 122, which was normal for him. His breath sounds were decreased throughout.
At approximately 2300 hours, he began to complain of increased shortness of breath. Chest physical examination revealed absent breath sounds on both sides with moderate to severe dyspnea. Heart rate was now between 140 and 150. SpO2 on the nasal cannula was 90% and dropping. A stat chest radiograph was nonrevealing. At this point, the tracheostomy was unplugged and the patient was placed on a tracheostomy collar connected to a large volume nebulizer set at 40%. In addition, an inner cannula was inserted into the tracheostomy tube and the patient was given several deep breaths with a manual resuscitator, lavaged with small boluses of normal saline, and suctioned. However, after several attempts, no mucus was removed and the patient’s condition continued to deteriorate. The patient was then given two aerosol treatments with 2.5 mg albuterol plus 2 mL of 20% acetylcysteine. At the end of the second treatment, the suction was repeated with the same negative results. At 2330, the patient’s heart rate was still around 150 and the SpO2 was now 88% on a 60% tracheostomy collar. The patient also was now obtunded.
Arterial blood gases were obtained with the following results: pH, 7.15; PaCO2, 125; PaO2, 116; HCO3, 49. The FiO2 on the tracheostomy collar was decreased to 40%. The patient’s attending physician and family were notified and were on their way to the hospital. Preparation was made to change the tracheostomy tube and to place the patient on ventilatory support. At this time, the patient began to have short runs of ventricular tachycardia.
However, at approximately 2350, the attending physician met with the family members. The result of this meeting was a decision to make EP a do-not-resuscitate and to keep him as comfortable as possible without any additional respiratory intervention. The patient was given lorazepam. The cardiac monitor was turned off, and the family gathered at the bedside to await EP’s death.
At approximately 0530, EP woke up and asked for a cup of coffee. After that, he continued to become more alert, and by that evening, his vital signs were back to what was normal for him. He indicated that he had no memory of what happened to him between 2345 and 0530. Over the next 7 days, he continued to improve and was transferred to a transitional hospital for rehabilitation.
There are many possible explanations for EP’s recovery without any active intervention. Certainly, most experienced respiratory therapists have been witness to similar patient situations. Thus, the real question that this case and others like it pose is: is there a lesson to be learned from it and, if so, what is that lesson?
William A. French, MA, RRT, is an associate professor at Lakeland Community College and a staff therapist at a local hospital in Kirtland, Ohio.