Preclinical testing of aerosolized mRNA formulations currently under development for the treatment of pneumonia-associated lung inflammation improved symptoms in a bacterial pneumonia model, according to Cambridge, Mass.-based biotechnology company Factor Bioscience Inc.
The study, published in Nucleic Acid Therapeutics, was led by Factor’s collaborator, Daniel O’Toole, PhD, senior research fellow, senior lecturer in lung regenerative medicine, and principal investigator in the CURAM and REMEDI institutes at the University of Galway.
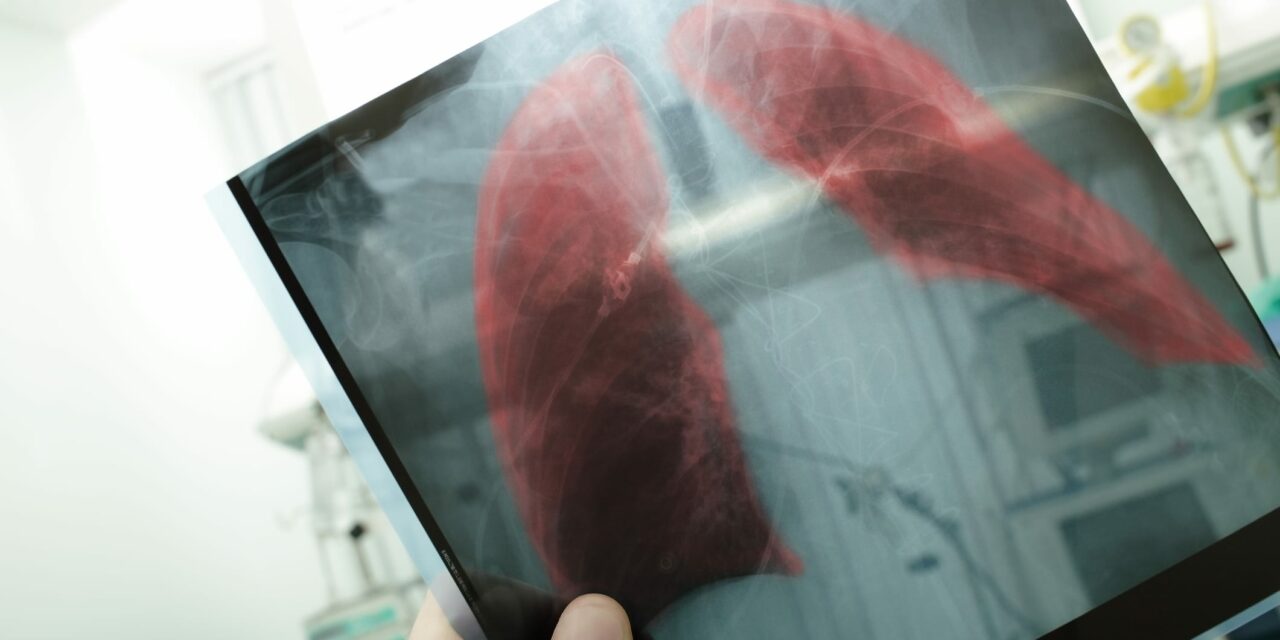
“Pneumonia is a debilitating disease in which infection causes inflammation of lung tissue, often leading to pulmonary edema and, in severe cases, acute respiratory distress syndrome (ARDS) and death,” says O’Toole in a press release. “There are currently no effective specific therapies for ARDS, and the mortality rate remains high. The ability to directly express anti-inflammatory proteins in lung tissue makes aerosolized mRNA an attractive candidate therapy for pneumonia. In particular, the speed with which cells express proteins when treated with mRNA is particularly important in the context of a rapid-onset disease such as ARDS.”
In previous studies, nuclear factor-κB inhibitor α super-repressor (IκBα-SR) and extracellular superoxide dismutase 3 (SOD3) reduced pneumonia severity when prophylactically delivered by viral vector.
In this study, mRNA coding for green fluorescent protein, IκBα-SR, or SOD3 was complexed with cationic lipid, passed through a vibrating mesh nebulizer, and delivered to cell culture or directly to rats undergoing Escherichia coli pneumonia. Injury level was then assessed at 48 hours. In vitro, expression was observed as early as four hours in lung epithelial cells.
IκBα-SR and wild-type IκBα mRNAs attenuated inflammatory markers, while SOD3 mRNA induced protective and antioxidant effects. In rat E. coli pneumonia, IκBα-SR mRNA reduced arterial carbon dioxide and reduced lung wet/dry ratio. SOD3 mRNA improved static lung compliance and alveolar-arterial oxygen gradient and decreased bronchoalveolar lavage (BAL) bacteria load. White cell infiltration and inflammatory cytokine concentrations in BAL and serum were reduced by both mRNA treatments compared to scrambled mRNA controls.
“These findings indicate nebulized mRNA therapeutics are a promising approach to ARDS therapy, with rapid expression of protein and observable amelioration of pneumonia symptoms,” according to the study.
The results are the latest in a long-standing collaboration between Factor and CURAM, the Science Foundation Ireland Centre for Research in Medical Devices. Factor and CURAM have multiple active collaborative projects, including projects focused on the development of mRNA-reprogrammed induced pluripotent stem cell-derived therapies for the treatment of pulmonary diseases as well as next-generation aerosolized mRNA vaccines.
“We are incredibly proud of our collaboration with CURAM and are excited about the results of this study,” says Christopher Rohde, PhD, chief technology officer of Factor, in a press release. “mRNA offers unmatched flexibility as a vector for expressing therapeutic proteins safely and reliably, and the results of this study support the use of aerosolized mRNA formulations for expression of therapeutic proteins in the lung. We are excited to continue this work with the team at CURAM and advance product candidates based on these results towards clinical development.”