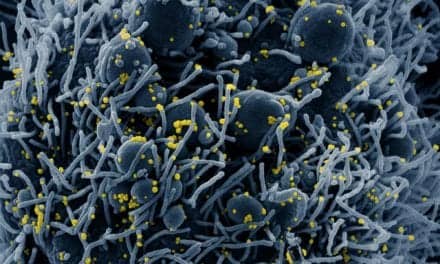
Data from three retrospective real-world studies showed that early administration of remdesivir (Veklury, Gilead Sciences) in hospitalized COVID-19 patients reduced mortality and hospital readmission rates, regardless of variant or disease severity.
The studies evaluated routine clinical practice data from over 800 hospitals throughout the US involving over 500,000 patients to gain insights on patient outcomes as COVID-19 continues to evolve over time. The data was presented at the 30th Conference on Retroviruses and Opportunistic Infections (CROI).
“Early treatment with remdesivir led to better patient outcomes regardless of the predominant circulating variant of concern. We see this risk reduction consistently across all oxygen levels and disease severity, including in immunocompromised patients. This is indeed a paradigm shift in the way we think about treating our most vulnerable patients,” says Chidinma Chima-Melton, MD, study author and pulmonologist at UCLA Health. “Large studies utilizing real-world clinical practice data are of great importance given the significant shifts that have occurred in the COVID-19 treatment landscape. These longitudinal analyses demonstrated the value of remdesivir in reducing mortality in all patients with COVID-19 and its positive impact on reducing readmission rates, which is an important consideration for hospitals.”
Mortality Outcomes in Patients Hospitalized with COVID-19
Two studies examined all-cause inpatient mortality rates at 14 and 28 days and demonstrated that initiation of remdesivir within the first two days of hospital admission was associated with a statistically significant lower risk for mortality in all oxygen levels compared to matched controls that did not receive remdesivir during their hospitalization for COVID-19.
For patients with no documented use of supplemental oxygen at baseline, treatment was associated with a 19% (p<0.001) lower risk of mortality at day 28. Patients on low-flow or high-flow oxygen also had a 21% (p<0.001) and 12% (p<0.001) lower risk of mortality at day 28, respectively. Patients on invasive mechanical ventilation/extracorporeal membrane oxygenation at baseline had a 26% (p<0.001) reduced risk for mortality at day 28.
These findings were observed throughout all variant time periods, including Omicron, in patients who did not require supplemental oxygen and across all levels of supplemental oxygen use, including those on invasive mechanical ventilation/extracorporeal membrane oxygenation.
The second analysis demonstrated that a reduction in mortality was also associated in vulnerable patient populations, such as patients with immunocompromised conditions, who can experience repeat infections and breakthrough infections. Results demonstrated that at day 28 mortality results showed that timely initiation of treatment within two days of hospital admission was associated with an overall 25% significantly lower risk compared to non-remdesivir across all variant time periods [pre-Delta (35%), Delta (21%), and Omicron (16%)].
Readmission in Patients Hospitalized with COVID-19
A separate analysis found that hospitalized patients with COVID-19 treated with remdesivir were also significantly less likely (27%) to be readmitted within 30 days to the same hospital. This finding was consistent across variant time periods of the pandemic. The lower rate of hospital readmission for patients treated with remdesivir was observed even in patients who had higher supplemental oxygen requirements during initial hospitalization for COVID-19.
Based on in vitro analyses presented at CROI, remdesivir retains potent antiviral activity against recent Omicron subvariants of concern, including XBB, BQ 1.1, BA.2.75, BA.4, BA 4.6, and BA.5. These data support the continued use of remdesivir to treat patients with Omicron subvariants of SARS-CoV-2.