Scientists have revealed that protracted lung inflammation following COVID-19 is strongly linked to long-term changes in lung structure and function, according to a report published in eLife.
The results suggest that monitoring people for markers of inflammation after infection with the SARS-CoV-2 virus could help identify those at risk of long-term lung problems and optimize follow-up care.
Although a vast majority of COVID-19 patients display mild disease, a significant proportion reports lingering or recurring clinical symptoms and full recovery can take several months to years.
“Symptoms lasting beyond 12 weeks are found in as many as 10% of COVID-19 patients and robust, resource-saving tools assessing people’s individual risk of lung complications are urgently needed,” says Thomas Sonnweber, a lung specialist at the Medical University of Innsbruck, Austria, and co-first author of the study alongside Piotr Tymoszuk. “We analyzed the frequency of lung structure and function changes and persistent symptoms in patients six months after a COVID-19 diagnosis, to investigate whether there are clinical hallmarks that can predict their risk of developing long COVID.”
The researchers evaluated the recovery of 145 primarily hospitalized patients diagnosed with COVID-19 between March and June 2020 who took part in the Austrian clinical study called ‘Development of Interstitial Lung Disease in COVID-19’ (CovILD).
They retrospectively assessed patient characteristics during their acute COVID-19 infection and then performed follow-up investigations at 60, 100 and 180 days. At each visit, they assessed symptoms and physical performance using a questionnaire, and conducted lung function tests, blood tests and a chest scan.
Almost half (49%) of patients had persistent complaints six months after diagnosis, with the most common complaints being impaired physical performance (34.7% of patients), sleep disorders (27.1%) and breathlessness on exertion (22.8%). Although the frequency of these symptoms declined as time passed, they were slower to resolve towards the end of the convalescence period, at the 100-day and 180-day follow-up visits.
Six months after diagnosis, a third of patients (33.6%) had impaired lung function and almost half of patients (48.5%) had chest scans showing structural lung abnormalities, with one in five patients (19.4%) having moderate-to-severe lung alterations.
To identify risk factors associated with these long-term problems, the team used machine learning algorithms to look for patterns of clinical features in the patients who had long COVID symptoms. They found that risk factors linked to severe and critical COVID-19 infection — namely being male, having long-term conditions such as high blood pressure, and high anti-SARS-CoV-2 antibody levels — were also linked to long-term symptom persistence. But in addition to these factors, elevated markers of inflammation — both body-wide and within blood vessels — were also associated with long-term lung abnormalities.
The team then tested if algorithms using these risk factors could predict COVID outcomes in a different group of patients. They found that although the inflammation markers predicted who would develop lung structure abnormalities, they could not accurately predict who would develop lung function problems or other symptoms such as breathlessness. This suggests that even if patients have detectable changes to their lungs 60 days after diagnosis, this may not manifest as symptoms or changes in lung function yet, but could still lead to problems later.
The algorithms need to be validated in larger groups of patients with COVID-19 before they can be reliably used to predict long-term COVID-19 outcomes. To this end, the authors have published their findings as an open-source risk assessment tool for other researchers to use.
“In our study group of patients, we found a high frequency of structural and functional lung abnormalities and persistent symptoms six months after a COVID-19 diagnosis, and a recovery trajectory that slowed after three months,” concludes Judith Löffler-Ragg, a lung specialist at the Medical University of Innsbruck, and co-senior author of the study alongside Ivan Tancevski. “Our risk models revealed a set of clinical measurements linked to lengthened recovery, independent to the severity of infection, which include known inflammatory markers. We hope that these could be used to identify those at risk of persistent lung problems and optimize their care to prevent long-term disability.”
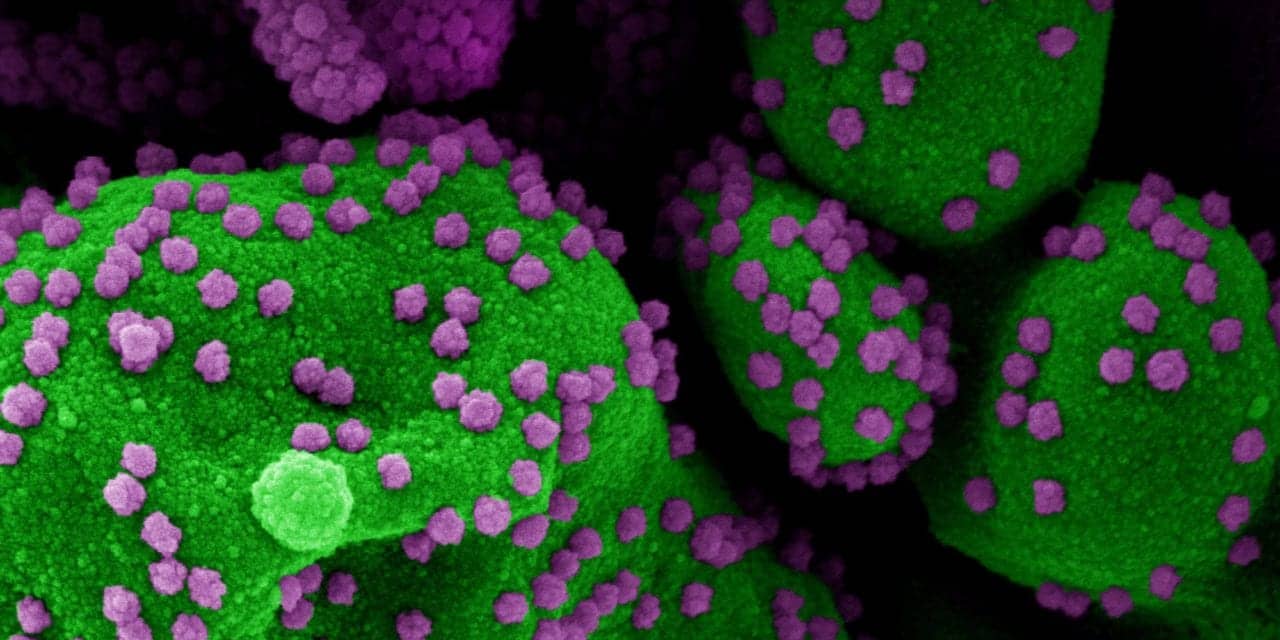
protracted lung inflammation