Disease of the small airways in the lungs is a potential long-lasting effect of COVID-19, according to a new study published in the journal Radiology. The study found that small airways disease occurred independently of initial infection severity. The long-term consequences are unknown.
Early reports indicate that more than 50% of adult survivors of SARS-CoV-2 infection experience post-acute sequelae of COVID-19 (PASC), more commonly known as “long COVID.” Respiratory symptoms, including cough and dyspnea, are reported by nearly 30% of patients with long COVID, including those who experienced mild infection.
The study grew out of observations from University of Iowa clinicians that many patients with initial SARS-CoV-2 infection who were either hospitalized or treated in the ambulatory setting later showed signs of chronic lung disease such as shortness of breath and other respiratory symptoms.
“There is some disease happening in the small airways independent of the severity of COVID-19,” said study senior author Alejandro P. Comellas, MD, professor of internal medicine and faculty in the Division of Pulmonary and Critical Care Medicine at the Carver College of Medicine, University of Iowa in Iowa City. “We need to investigate further to see whether it is transient or more permanent.”
Dr. Comellas and colleagues put a protocol in place to perform both inspiratory and expiratory CT in these patients. Inspiratory CT, performed after patients inhale, is the standard imaging technique for viewing lung tissue, but post-exhalation expiratory scans are needed to assess air trapping, a condition in which people are not able to empty their lungs when they breathe out. Air trapping is found in many obstructive airway diseases, such as asthma and chronic obstructive pulmonary disease (COPD).
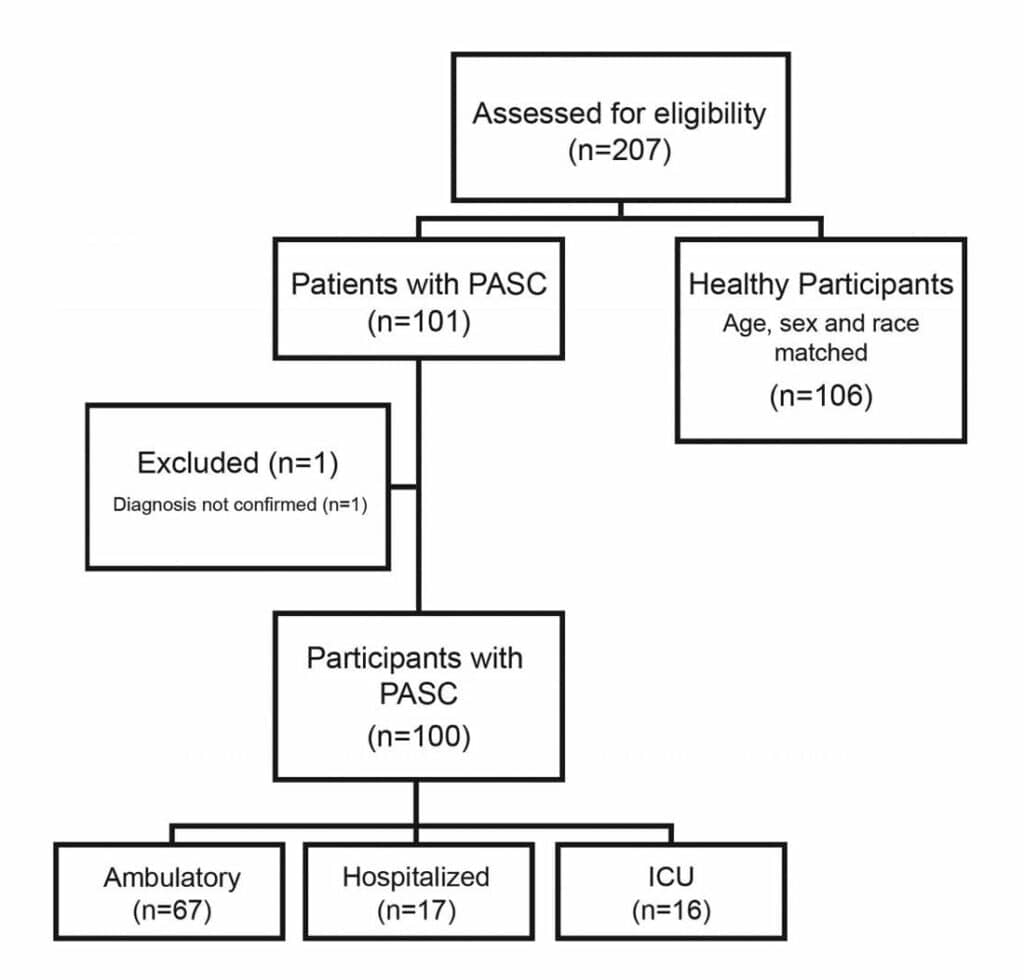
For the study, the researchers compared CT findings in people who had COVID-19 and persistent symptoms with those of a healthy control group. They enrolled 100 adults with confirmed COVID-19 who had remained symptomatic more than 30 days following diagnosis, along with 106 healthy participants. The 100 COVID-19 survivors, median age 48 years, included 67 who were classified as ambulatory, or not requiring hospitalization, 17 who were hospitalized, and 16 who required care in the intensive care unit (ICU) during acute infection.
The researchers detected air trapping on expiratory chest CT images in the COVID-19 group. The mean percentage of total lung affected by air trapping ranged from slightly more than 25% in the ambulatory group to almost 35% in the hospitalized group, compared with only 7.2% in healthy controls. Air trapping persisted in eight of the nine participants who underwent imaging more than 200 days after diagnosis.
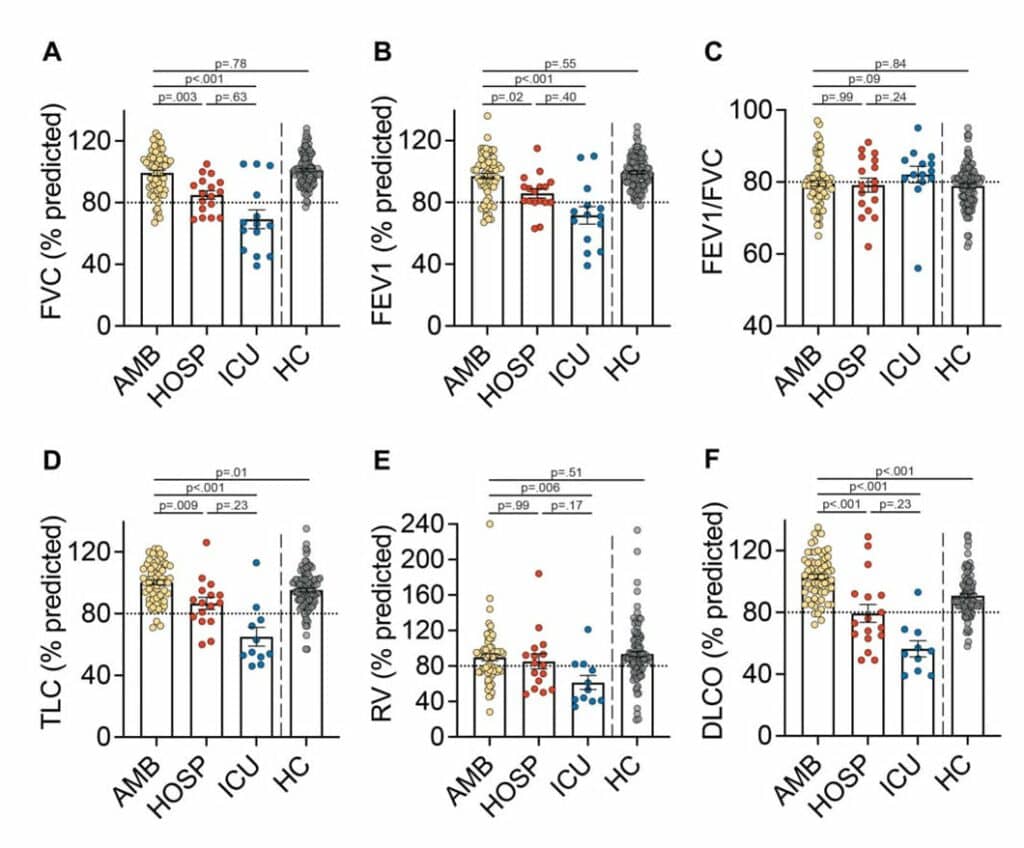
These imaging results show a high prevalence of long-lasting air trapping, regardless of the initial severity of infection.
Quantitative analysis of expiratory chest CT images, performed with the help of a sophisticated type of artificial intelligence known as supervised machine learning, showed evidence of small airways disease. While small airways disease is not fully understood, evidence suggests it may be related to either inflammation or remodeling of the small airways that prevents air from being able to be exhaled from the lungs.
“For the first time, we’re describing small airways disease in this population of COVID-19 patients with persistent symptoms,” Dr. Comellas said. “Something is going on in the distal airways related to either inflammation or fibrosis that is giving us a signal of air trapping.”

The median time from diagnosis to chest CT imaging was approximately 75 days. The researchers noted that persistence of respiratory abnormalities in this timeframe raises concern for permanent airway remodeling and fibrosis following SARS-CoV-2 infection.
Dr. Comellas and colleagues intend to follow the patients in the study registry and see how many improve and recover and how many remain with abnormal findings.
“If a portion of patients continues to have small airways disease, then we need to think about the mechanisms behind it,” he said. “It could be something related to inflammation that’s reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease.”
long covid small airways disease