Cytokine interleukin-22 (IL-22), a human genetic protein, is required for normal lung repair after influenza infection, a finding that represents “a novel pathway involved in interstitial lung disease,” according to the results of a new study published in The American Journal of Pathology.
“We demonstrate that IL-22 plays a critical role in regulating pulmonary epithelial repair responses during influenza infection and resolution,” says Dr. Alcorn. IL-22 is currently under development as a potential therapeutic in human clinical trials.
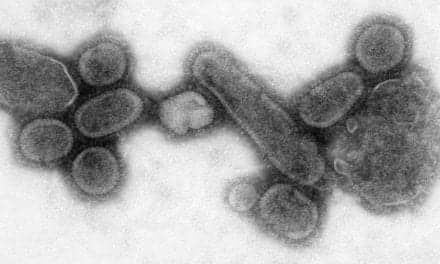
In a series of experiments, researchers infected 6- to 8-week-old wild-type (WT) mice (C57BL/6 strain) and IL-22-deficient mice with either influenza A PR/8/34 H1N1 or a control vehicle. They discovered that in WT mice not infected with influenza, IL-22 receptors were distributed on epithelial cells of the large and small airways, but not within the parenchyma. According to researchers, this receptor distribution suggests that, in the absence of lung injury, IL-22 interacts mainly with the bronchial epithelial cells.
Three weeks following influenza infection, IL-22 receptors were observed in parenchymal tissue in injured areas, such as alveoli under repair. Researchers suggest the IL-22 receptor can be upregulated at sites of influenza-associated injury.
Ten days following infection, IL-22-deficient mice showed significantly more severe damage and greater lung edema than WT control mice. No differences were found in viral load. In addition to an increase in the number of lymphocytes in the IL-22-deficient animals, the IL-22-deficient mice also showed functional impairments such as significantly decreased compliance and increased hysteresis. fee
“With the increasing prevalence of more infective and/or virulent strains of influenza, understanding the impact of virus on the host epithelium and the processes involved in lung repair are of great importance,” says John F. Alcorn, PhD, an immunologist affiliated with the department of pediatrics at the Children’s Hospital of Pittsburgh of UPMC.
Alcorn noted that the findings open up new possibilities for developing therapeutic agents that promote recovery of normal lung function and architecture after influenza infection and lessen the likelihood of secondary infections. “A key finding is that even after the resolution of infection, influenza results in lung parenchymal remodeling that may be critical to susceptibility to further injury.”