
Respiratory failure due to hypoxemia and/or hypercapnia calls for oxygen therapy, positive pressure support, and possibly ventilatory support. Care for these patients may escalate and require higher flow, FiO2, and more complex devices and intensive monitoring.
By Bill Pruitt, MBA, RRT, CPFT, AE-C, FAARC
Published: March, 19, 2021
Respiratory failure occurs when there is a failure of the pulmonary system in one or both of its two main functions which occur at the alveolar level but depend on the entire system to work properly. These main functions are oxygenation of the blood and/or removal of carbon dioxide (CO2) from the blood.1
Hypoxemic respiratory failure (abnormally low PaO2) results from issues such as pulmonary edema, infection/pneumonia, ARDS, atelectasis, trauma, and more recently in patients with SARS-CoV-2 coronavirus infection or COVID-19. These conditions interfere with the ability of oxygen to move from the alveoli into the blood stream. Hypercapnic (abnormally high PaCO2) respiratory failure, often referred to as pump failure, is a problem with getting CO2 cleared from the body.2 This is due to ineffective ventilation as a result of increased airway obstruction, defects in the chest wall, neurologic issues, or weakness in the respiratory muscles.

These problems can be a result of inflammation, retained secretions, flail chest, decreased ventilatory drive, fatigue, or a flattened diaphragm from air-trapping/hyperinflation (causing ineffective or inefficient movement). COPD, obesity-hypoventilation, and pneumonia are frequently associated with hypoxemic respiratory failure and (if the failure state or condition is prolonged or severe) can also include hypercapnic respiratory failure.3
Stepping Up in Levels of Care: Hypoxemic Respiratory Failure
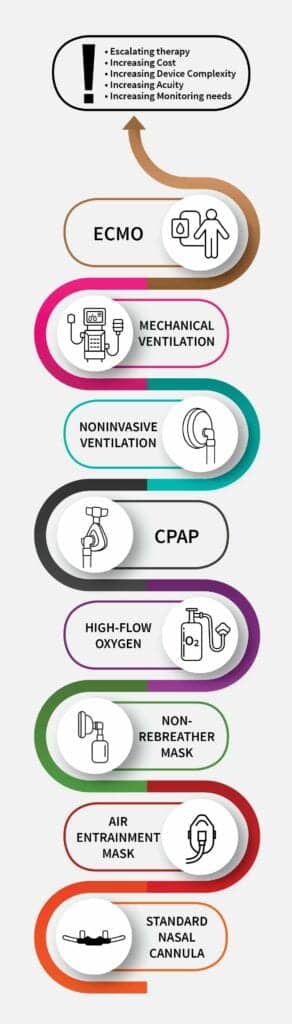
For hypoxemic respiratory failure, oxygen therapy is the first and primary treatment strategy. Oxygen therapy provides supplemental oxygen and can be delivered by several means. O2 delivery often occurs starting with a simple nasal cannula. If not sufficient to correct the hypoxemia, the next steps (in order of increased flow delivery and/or FiO2 ) include the air-entrainment mask, and non-rebreather mask.4 A patient’s inspiratory demand and inspiratory flow often exceeds the flow delivery of these devices so room air is mixed in with the oxygen diluting the FiO2. All of these approaches to oxygen therapy involve disposable, single-use devices.
The next step up to treat continuing hypoxemia and hypoxic respiratory failure is a high-flow nasal cannula (referred to as HFNC or high-flow oxygen therapy, HFT). This requires a more complex system than the previously mentioned devices. This includes a high-flow nasal cannula, a high-flow source with systems regulating the flow and the FiO2, a humidifier system, and heated tubing.5 This system provides high-flow (30 to 60 LPM) oxygen that is heated to body temperature (37oC) and is fully saturated (100% relative humidity) with minimal or no rainout in the tubing.
The advantages of this delivery system are:
- Reduced or elimination of dilution of the inspired oxygen with room air
- Washout of deadspace in the airways
- Increased tidal volume
- Generation of low-level continuous positive airway pressure (CPAP)
- Increased patient comfort and adherence to the therapy, and
- Improved mucociliary transport.5
Continuous positive airway pressure (CPAP) and noninvasive ventilation (NIV) using bilevel intermittent positive air pressure (BiPAP) have proven to be an effective and safe strategy to treat hypoxemic respiratory failure due to cardiogenic pulmonary edema.6,7 CPAP provides a constant state of positive pressure in the airways (ie, 5 cmH2O), increases functional residual capacity (FRC) and includes the capacity of adding supplemental oxygen. As a result, some areas of atelectasis will be recruited to become functional and the tendency for areas to become atelectatic will be greatly hindered or stopped. This improves oxygenation. BiPAP uses a baseline positive pressure (expiratory positive airway pressure or EPAP—ie, 5 cm H2O) and upon inspiration, pressurizes the system using pressure support to a higher positive pressure (inspiratory positive airway pressure or IPAP—ie, 10 cmH2O). BiPAP can also provide supplemental oxygen.
In patients with other causes for hypoxemic respiratory failure beyond cardiogenic pulmonary edema, studies on BiPAP have shown a mixed outcome. The most often used interface for BiPAP is a face mask but there may be a problem with higher than desired delivered tidal volumes and subsequent ventilator-induced lung injury.8,9 However, studies using a helmet as the interface for BiPAP have shown that lower levels of pressure support and lower tidal volumes are the result, which favors lung protective strategies.8
[Adapted from Scala R, et al #10]
Stepping Up in Levels of Care: Hypercapnic Respiratory Failure
Treatment for hypercapnic respiratory failure frequently uses BiPAP, especially in patients with COPD exacerbation or cardiogenic pulmonary edema. The EPAP setting offers the same positive effects as previously discussed in relation to CPAP. EPAP is titrated to improve oxygenation and address atelectasis. The IPAP setting utilizes pressure support to improve ventilation, unload the respiratory muscles, and reduce PaCO2.9
There are some published studies comparing the use of HFT to BiPAP in exacerbation of COPD with hypercapnic respiratory failure that conclude that either of these treatment strategies can be used. The argument for using HFT in this setting includes two factors: first is that HFT washes out deadspace, the second is that HFT provides more humidity and may be better in secretion clearance as a result.9 If the treatment for hypoxemic or hypercapnic respiratory failure using HFNC, CPAP, or BiPAP have not been successful or not tolerated, the next step is to intubate and institute mechanical ventilation.
The final strategy for the most critically ill patient who has moved through all the previous steps is to use extracorporeal membrane oxygenation (ECMO). Moving through these steps involves escalating therapy with increasing cost, device complexity, acuity, and monitoring needs. (See Figure 1: Escalating Support.)10
COVID-19 Issues
COVID-19 frequently causes hypoxemic respiratory failure due to viral pneumonia and ARDS in those patients admitted to the ICU. Use of HFT, CPAP, and BiPAP is often used in a stepwise fashion to find the lowest effective support and aim to avoid intubation if possible. The World Health Organization (WHO) guidelines for managing critically ill adults with COVID-19 recommend using NIV in select patients with hypoxemic respiratory failure who can be closely monitored by experienced medical staff. Intubation and mechanical ventilation must be readily available in cases of rapid deterioration or in those who show no improvement after a short trial period. The United Kingdom’s National Health Service recommends using NIV as the first step in managing patients with hypoxemic acute respiratory failure, with similar recommendations coming out from Italy, Spain, and Russia.11
Infection Control in COVID-19 Cases
Several recommendations have been published to reduce possible infection of COVID-19 for healthcare workers.12 Use of personal protective equipment are the first line of defense. This includes a high-efficacy N95 mask, integral-frame protective goggles, gloves, and long-sleeved impermeable microbiological protective gowns. Next, patients should be placed in negative pressure rooms or (if not available) a single-patient room with bathroom and doors should be closed at all times. For in-house transport, the patient should wear a surgical mask. For HFT patients, staff should keep a distance of six feet from the patient (as much as possible) and the patient should wear a surgical mask over the HFNC.12
For NIV and BiPAP circuits, a high-efficiency and low-resistance antimicrobial filter should be placed on the exhalation port. If a filter cannot be placed on the expiratory port, it should be inserted between the patient connection and the device tubing, with extra monitoring and response to increased resistance (the filter may need frequent changes) Heat and moisture exchangers (HMEs) should not be used. For the patient interface, a helmet or full-face mask is preferred. If not available, then an oronasal mask should be used. Leaks need to be minimized to avoid exposure to infected exhaled air. A nasal mask should not be used due to issues with increased generation of aerosols.
For inhaled medications, metered dose inhalers (MDI) are preferred. Nebulizers generate aerosols and should be used only if the medication is not available in an MDI, if the patient is uncooperative or unable to follow instructions for using an MDI, or if the patient has a poor response to the MDI. If a nebulizer is needed a vibrating mesh should be used.12
Utilizing One Device for Several Modalities: The Philips V60 Plus
Patients suffering from acute respiratory failure (hypoxemic and/or hypercapnic) move through the steps outlined above, sometimes with a rapid escalation of acuity and increasing need for more intense support over a short time period. As a patient improves, care often steps down but a setback or deterioration in the patient’s condition frequently calls for a return to the higher step.
At the level of care calling for CPAP, HFT, or BiPAP, or invasive mechanical ventilation, the Philips V60 Plus ventilator can be used to provide all of these modalities in one device. (Note: V60 units can be upgraded to include HFT to provide this additional mode.)
Time Savings in Escalating Care
The capacity of the V60 Plus to move from one supportive strategy to the next has many advantages. It eliminates the time needed to obtain and setup another device which often involves leaving the ICU to go to the equipment storage area, return with the device, install the circuit, connect to power and gas supply, check the settings, remove the patient from the device in use and connect the new one, verify settings and alarms.
“Offering both NIV and HFT on the same ventilator can save time and limit disruption. In market research, the process of obtaining an HFT device, moving it into the patient room, preparing it for therapy delivery and completing patient set-up consumed 16.3 minutes on average, as compared to an average of only 3.8 minutes with the V60 Plus.”13
Time is also reduced when a device is no longer needed. With a V60 Plus, cleaning and setup only occurs with the single device compared with time needed to clean and setup multiple devices. When dedicated devices are utilized, often one or more devices needs to left in the room on stand-by. This adds to the already crowded conditions often found in the ICU setting.
Cost Savings in Escalating Care
The V60 Plus saves the cost that would otherwise be incurred by having separate, dedicated systems such as a HFT device, a BiPAP device, and a mechanical ventilator. When dedicated devices are utilized, often one or more devices needs to left in the room on stand-by. This adds to the already crowded conditions often found in the ICU setting. Using the V60 Plus also saves room in the equipment storage area by eliminating the need for additional space with dedicated devices. Moreover, the single-arm heated circuit can be used with both HFT and NIV, which is another cost savings (the only change needed is the patient interface).
V60 Plus Features
The V60 Plus offers HFT, average volume-assured pressure support (AVAPS, which targets a tidal volume using a pressure-limited approach to titrate the delivered volume over several breaths), Pressure Control Ventilation (PCV), and CPAP with the C-Flex option, which offers three levels of flow-based expiratory pressure relief. With this capability the V60 Plus can provide both non-invasive and invasive ventilation for adults and pediatric patients (>20 kg).
The V60 Plus offers all the features of a critical care ventilator in the alarms package and the optional settings needed to adjust inspiration and expiration for patient comfort. Mode selections include CPAP, PCV, AVAPS, PPV, and HFT. Settings include tidal volume, rate, inspiratory time, rise time, EPAP, minimum and maximum inspiratory pressure, FiO2, 100% O2 key to use for suctioning, an alarm silence key, and alarm reset key. The alarm package includes high and low respiratory rate, high and low tidal volume, high and low inspiratory pressure, low minute volume, and low inspiratory pressure (time). The low rate alarm also serves as an apnea alarm and a backup rate will be initiated provided the low rate alarm is set higher than the backup rate but lower than the patient’s spontaneous rate. The patient data display includes rate, estimated tidal volume, estimated minute ventilation, peak inspiratory pressure, patient trigger %, inspiratory time/total cycle time % (TI/Ttot%) and leak. The Mask/Port menu button allow the clinical staff to choose various mask leak values and to choose the correct port. The breath-type indicator color on the patient display corresponds to waveform color: turquoise for spontaneously triggered breaths, orange for timed triggered breaths, and blue for exhalation.
Transport Capability
Another advantage of the V60 Plus is that the device can be utilized for transport (with the addition of an oxygen cylinder) which provides continuous support. This prevents the possible deterioration in the patient’s condition that can come from changing to a transport ventilator, simple oxygen set-up, or manual ventilation with a resuscitator bag approach.
Conclusion
Respiratory failure due to hypoxemia and/or hypercapnia calls for oxygen therapy, positive pressure support, and possibly ventilatory support. Care for these patients may escalate and require higher flow, FiO2, and more complex, expensive devices with more intensive monitoring and higher cost. The Philips V60 Plus provides several treatment strategies in one device, which can save time and cost while providing convenience, quick changes between modalities, excellent monitoring and alarms, and safety, with the capacity to move with the patient when needed for transport.
RT
Bill Pruitt, MBA, RRT, CPFT, AE-C, FAARC, is a writer, lecturer, and consultant and recently retired from over 20 years teaching at the University of South Alabama in Cardiorespiratory Care. He also volunteers at the Pulmonary Clinic at Victory Health Partners in Mobile, AL.
For more information, contact [email protected].
References
- Frat JP, Coudroy R, Thille AW. Noninvasive ventilation or high‐flow oxygen therapy: When to choose one over the other? Respirology. 2019 Aug;24(8):724-31.
- Roussos CH. The failing ventilatory pump. Lung. 1982 Dec;160(1):59-84.
- Roussos C, Koutsoukou A. Respiratory failure. European Respiratory Journal. 2003 Nov 16;22(47 suppl):3s-14s.
- Heuer, A. Medical Gas Therapy In: Kacmarek R, Stoller J, Heuer A. Egan’s Fundamentals of Respiratory Care. 11th ed. St. Louis, MO: Elsevier; 2017: 514-539.
- Masclans JR, Pérez-Terán P, Roca O. The role of high-flow oxygen therapy in acute respiratory failure. Medicina Intensiva (English Edition). 2015 Nov 1;39(8):505-15.
- Hess DR. Should noninvasive ventilation be used for treatment of acute cardiogenic pulmonary edema? A Cochrane Review summary with commentary. Respiratory care. 2020 Apr 1;65(4):573-4.
- From Peraino, T. “Evidence-based practice for non-invasive ventilation and high flow nasal cannula: a summary of the literature.” in Philips HFT-therapy-clinical-summary.pdf Accessed 3/10/21.
- Frat JP, Coudroy R, Marjanovic N, Thille AW. High-flow nasal oxygen therapy and noninvasive ventilation in the management of acute hypoxemic respiratory failure. Annals of translational medicine. 2017 Jul;5(14).
- Koga Y, Kaneda K, Fujii N, Tanaka R, Miyauchi T, Fujita M, Hidaka K, Oda Y, Tsuruta R. Comparison of high‐flow nasal cannula oxygen therapy and non‐invasive ventilation as first‐line therapy in respiratory failure: a multicenter retrospective study. Acute medicine & surgery. 2020 Jan;7(1):e461.
- Scala R, Heunks L. Highlights in acute respiratory failure. European Respiratory Review 2018 27: 180008; DOI: 10.1183/16000617.0008-2018
- Avdeev SN. Non-invasive ventilation in patients with novel coronavirus infection COVID-19. Scientific and practical journal PUL’MONOLOGIYA. 2020 Jan 1:679.
- Gómez, C.C., Rodríguez, Ó.P., Torné, M.L., Santaolalla, C.E., Jiménez, J.F.M., et al. 2020. Clinical consensus recommendations regarding non-invasive respiratory support in the adult patient with acute respiratory failure secondary to SARS-CoV-2 infection. Medicina Intensiva (English Edition), 44(7), pp.429-438.
- Formative testing report. Philips V60 Product Testing, Results and Recommendations. ResearchWorks May 31, 2017.









