The need for fast, accurate sleep testing is greater than ever, but whether or not home-based testing is the answer is still under debate.
In a recent study to determine the prevalence of sleep apnea in the general population, it was determined that even among adults who had access to a sleep clinic, at least 80 percent with moderate to severe sleep apnea had not been diagnosed.1 Although the knowledge of sleep-disordered breathing (SDB) among the medical community has grown substantially in the past several years, the above figure would seem to indicate there is still a great need to find a cost-effective and timely way to test sleep-
disordered individuals.
Traditionally, sleep studies have been conducted in a laboratory using diagnostic equipment and video cameras.2 The limited number of laboratory facilities, however, means it is difficult to diagnose everybody with SDB in a timely fashion.2 One alternative that has been growing in popularity in recent years is home-based sleep studies. Mention the subject to professionals in the sleep field, however, and you are sure to spark a passionate debate as to whether home studies are as effective as those done in the sleep laboratory.
“I don’t want to appear to be a stick in the mud about home sleep testing, because there’s always room for progress,” says Ralph Downey III, PhD, director of the Sleep Medicine Department at Loma Linda VA Medical Center and Loma Linda University Medical Center, Loma Linda, Calif. “But practically speaking, because we do split-night studies for most SDB patients, I don’t see any significant benefit to changing what we’re doing in the sleep lab at this point.”
As far as home testing is concerned, says Pamela Minkley, RRT, CPFT, RPSGT, of Ingham Regional Sleep/Wake Center, Lansing, Mich, “it makes sense to assume that for it to compete with the results of testing conducted in a sleep lab, the associated technology also must keep pace. Compared with the early days of home sleep testing nearly 2 decades ago, however, today’s home-testing technology improves almost on a daily basis, and comes fairly close for specific types of testing. Clearly, we can provide adequate home-based testing, technologically speaking.”
Testing At Home
“A home sleep study could be as simple as putting an oximeter on the patient’s finger and monitoring oximetry overnight, on up to full polysomnography, where you have complete raw data information about an EEG [electroencephalogram],” says Robert Turner, RRT, RPSGT, manager and clinician at Rose Sleep Disorders Center, Denver.
A four-channel cardiorespiratory study can potentially be done more cost-effectively in a patient’s home.2 One problem with this type of unattended study, however, is that data may be lost because of equipment failures or environmental factors, requiring a repeat test. Also, there is only a limited amount of information that can be obtained from this type of study. In addition, most home studies do not measure total sleep time, so they may underestimate the severity of apnea.2
Minkley believes the real question of whether home and lab testing can be used interchangeably revolves around the goals of home-based sleep testing. “In order for home-based testing to succeed, you have to match the study goals with available technology, and you have to consider whether patient intervention is necessary, either to initiate therapy or maintain the recording, or for patient safety.” Not all patients will benefit from home-based testing, but in many situations, the home offers a solid alternative, Minkley says.
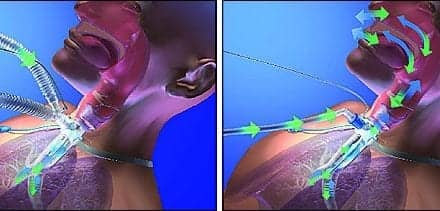
“The question is, when is a simple diagnostic test better?” Turner says. The clinician must decide when to use home testing on a case-by-case basis (Figure 1, page 56).
“Generally, patients who benefit from home testing are not severe enough for intervention, but just need a study recorded all night, uninterrupted,” Minkley says. Such testing could prove useful, for example, in evaluating an SDB patient’s current therapy, she says. According to Turner, home testing can also be useful for patients who live in outlying rural areas who cannot easily reach a sleep center or for patients who are initially reluctant to seek treatment.
If it is determined that a patient does not have sleep apnea on the basis of a home study, Turner says, he or she most likely belongs in a sleep laboratory where technician monitoring can prove beneficial in identifying the problem; home monitoring devices still tend to focus only on the respiratory aspects of sleep problems. Other problems such as upper airway resistance syndrome (UARS) are difficult to identify if EEG data are not available. If a patient is sleepy and does not have sleep apnea according to a home study, that should not be the end point in the evaluation.
Other patients who are not appropriate for home sleep testing include those with parasomnias, who require close documented observation for accurate diagnosis; those who require a full study with extended electrode placements and observation, such as seizure patients; those with complicated respiratory problems; and those coming off a ventilator or who have a tracheotomy tube.
Minkley believes certain types of home testing can benefit even patients with complicated sleep disorders if it is carefully integrated into their testing and monitoring plans. For example, using video monitoring in a patient’s home before having him or her come into the center allows the technician to select the appropriate technology for the lab-based study, she says. Home video monitoring can help to better define a complicated parasomnia before a laboratory study is scheduled, Minkley says.
Patient education plays a primary role in the efficacy of home-based testing. Therefore, tests that require significant follow-up or patient training may not transfer well to the home setting, Turner says. “Some devices allow you to do CPAP titration in the home, but a lot of [sleep centers] are not doing that yet because, while the technical side of it is fine, on the titration side, helping the patient understand how the mask fits, how to fix leaks–those kinds of things is hard to do from a remote location,” he says.
Consumer Interest
Ideally, the answer to the home- versus lab-based sleep testing dilemma must come from the patients themselves, Downey says. “It should be patient-driven, not technology driven,” he says. “So far, though, the studies that I have seen have not shown an overwhelming propensity for people to want home studies. One simple argument is that I’m not sure they want people in the house; I’m not sure they want technology in the house.” At Loma Linda, he says, few patients even ask about home-based testing. This is a trend seen at other sleep centers as well. Rose Sleep Disorders Center actually discontinued its trial home-based testing program because of a lack of consumer demand.
For both insurers and patients, recent changes in lab-based testing approaches have rendered home-based testing a less appealing alternative. At Rose, as at many sleep centers nationwide, lab-based testing has shifted to a split-study style that allows the center to place a patient on CPAP during the second portion of the test the same evening. Turner says this approach can hamper effective implementation of home-based testing because it makes it difficult to measure in terms of cost to the insurer and long-run convenience to the patient. “From an economic standpoint, CPAP titration alone after the patient has had a home study costs the same as doing the diagnostic and the CPAP in a split fashion [at the lab],” he notes.
With newer “smart” autotitrating systems, he says, a patient could undergo testing at home and then be placed on an autotitrating CPAP device, similar to lab-based split testing. “Unfortunately, right now there’s some hesitation about using these devices because it’s difficult to know which one is going to work the best for patients. Some patients respond to one manufacturer’s device while another patient might respond to a different manufacturer’s device.” Once again, cost limits home-
testing applicability because currently, autotitrating systems are more expensive than the lab-based alternative.
Relying On The Evidence
In the past, researchers who used home-based testing had in mind a specific question, a specific study population, and equipment designed to record only the needed variables, Minkley says. “Now that home-based testing is more universally accepted, the issue has broadened to full diagnostic screening. How can we match the diagnostic and therapeutic goals of a sleep study with available technology in a cost-effective manner?” she says.
The future of home-based testing rests in large part on the ability of researchers to answer that question. Many sleep technologists, Downey included, are not convinced of the benefits, safety, and general efficacy of conducting sleep studies in the home. “The problem is, what is the gold standard? The gold standard thus far has been the sleep center,” Downey says. “I’m not sure a gold standard has been identified yet in the home.”
To achieve a level of professional comfort with the efficacy of home-based testing, Downey would like to see studies with results that favorably compare home studies to those conducted in the sleep center.
“The problem with that, of course, is that just because they differ may not mean that one is right and one is wrong. Whenever you do these types of studies, you necessarily change the gold standard,” he says. Home-based testing still lacks large, broad-based studies comparing the sleep of a population sample both in the home and in the lab. Such samples could reveal any potential differences attributable to the home environment monitoring situation and not necessarily to the methodology used, Downey says.
Technologists And Providers
Both in the lab and at home, health care providers ultimately determine the success of a sleep test. “I would always prefer a well-trained technologist who knows what they’re doing, using old technology, along with an interpreting physician who understands the technology, than a more technologically advanced system combined with someone who doesn’t understand the technology,” Turner says.
Successful sleep technicians who work in the home must meet higher training standards than do their counterparts who perform lab-based tests. “[Technicians in the home] have to be even better in terms of setting up the patient and ensuring the quality of the recording because they’re dealing with an uncontrolled environment–kids, cats, etc,” Downey notes. He worries that a greater emphasis on home testing will result in fewer monitored sessions and a corresponding drop in testing efficacy. “I find it invaluable that RCPs are constantly
monitoring the study,” he says. “It really gives life to that study when we review it. It’s one thing to review raw data–it’s all well and good and scientific–it’s another thing to review that raw data in terms of what the technician hears, sees, and knows about the patient because they’re interacting with him. Whenever you get more distant from that, you get more distant from an ideal diagnostic situation.”
Recently, education aimed at primary care providers has moved to the forefront. “Now that sleep apnea is fairly well recognized by primary care practitioners, demand for testing and availability of technology has increased at a very steep rate, much steeper than we’re able to increase medical education,” Minkley says. The growing emphasis on understanding sleep disorders, combined with primary care’s increasing prevalence throughout the health care industry, has resulted in more
sleep patients who receive care directed by a primary care physician. “Our ideal would be that our medical director would see everybody, but that’s not the reality of what happens,” Turner says. As a result, sleep centers like Rose provide primary care physicians with both formal and informal education so they have more up-to-date information about sleep medicine on which to base their decisions.
The Good With The Bad
Home-based sleep testing offers benefits to the overall sleep medicine community, but controversy remains. “The assumption made in the home is that it’s the natural environment, but the natural environment is often disruptive,” Downey says. “For example, a person may have a dog at home that sleeps with them. Well, maybe they don’t let the dog sleep with them on that night because they have the wires [on] and they don’t want to mess the study up,” Downey points out. Discovering these environmental sleep disruptions via appropriate questioning in the sleep center can sometimes be difficult, but working in the home also offers no guarantee that the testing process will identify them.
One true advantage of home-based sleep testing is that it expands the range of options sleep centers have available to them to diagnose and treat patients, Minkley says. “When home-based testing first emerged, I think some in the sleep community worried it would be the death of sleep centers,” she says. “On the contrary, as more individuals in the general public recognize sleep disorders, the industry is evolving to
Even hesitant sleep medicine professionals agree that home-based testing has the potential to strengthen sleep medicine, provided that it is used with caution. “It’s always good that people are looking for new ways to do sleep studies, and potentially less expensive ways, and seeking to get the same results,” Downey says. “However, I’m always leery that people confuse new technology with progress.”
Kathryn Olson is a contributing writer for RT.
References
1. Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20:705-706.
2. Millman RP. Home test or in-laboratory studies. Wake-Up Call: The Wellness Letter for Snoring and Apnea. Washington, DC: American Sleep Apnea Association; April/May 1997.