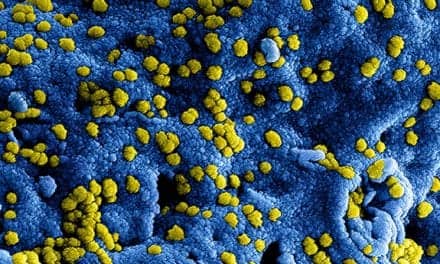
An infection pathway in the Pseudomonas aeruginosa bacterium, which has a widespread resistance to many antibiotics, is activated when the bug encounters low-oxygen conditions, according to University of Cambridge researchers.
This is of particular importance, the researchers believe, because “the bug is strongly associated with infections in patients with severe respiratory disease,” including cystic fibrosis.
When P. aeruginosa encounters low oxygen conditions, a mechanism called the Type III Secretion System (T3SS) is triggered. The T3SS resembles a molecular-scale ‘hypodermic syringe’ which is thought to inject toxins directly from the bacterium into the host cell, where they subvert its function and lead to cell death, according to researchers.
The team identified a metabolic ‘switch’ regulating T3SS activity, called the glyoxylate shunt, which is activated when oxygen is sparse. When this ‘switch’ is turned on an enzyme called isocitrate lyase (ICL) is expressed, leading to activation of the T3SS. In the absence of ICL, the T3SS is not turned on in low-oxygen conditions.
“Crucially we found that this regulatory pathway also affected the formation of antibiotic-resistant biofilms by P. aeruginosa,” said lead investigator Martin Welch, from the University of Cambridge Department of Biochemistry. “This is important because biofilm formation is known to play an important role in the pathology of cystic fibrosis-associated infections. Our study therefore opens up new potential avenues for the development of novel antibacterial therapeutic interventions.”