Airway clearance therapy adherence for adults can be complicated by a variety of factors, but pediatric patients face additional barriers to proper management simply due to their age.
Following doctor’s orders is essential for recovery, healing, and maintaining optimal quality of life. But for people with chronic respiratory conditions, this task can be complicated by a variety of factors, including a lack of knowledge, lifestyle barriers, or quite simply misunderstanding how to follow a particular therapy plan. For example, 70% of participants with cystic fibrosis (CF) in a Global Pediatric Health study said they forgot or failed to take their treatment (Shakkottai and Nasr 2017) and in general, reports of people with chronic conditions indicate only 30% to 70% are compliant (Meichenbaum 1987).
Why does adherence matter for condition management?
Recent research has demonstrated the importance of adherence for patients with chronic respiratory conditions. More specifically:
- Poor adherence with respiratory therapy is expensive, undermines the quality of life, can lead to antibiotic-related adverse events such as allergy and renal failure, and reduces life expectancy (Kettler 2002);
- A large population study showed that people with CF who possessed lower amounts of medication were significantly more likely to be admitted to the hospital for pulmonary exacerbation, and incur a greater need for IV antibiotics (Eakin 2011);
- In regard to inhaled treatments, patients who received four or more courses per year
of nebulized tobramycin were 60% less likely to be admitted to the hospital than those receiving only one (Briesacher 2011).
For pediatric patients, there are additional barriers to proper airway management and adherence simply because of their age. To overcome these barriers and improve care management and eventually outcomes, health care systems are increasingly turning to digital solutions. Digitally connected solutions, such as smart inhalers and Bluetooth-enabled devices, help create a coordinated, connected system among manufacturers, care providers, caregivers and other parties involved in a child’s care.
The following are three things respiratory therapists can do to build a successful pediatric monitoring program that leads to better adherence and outcomes.
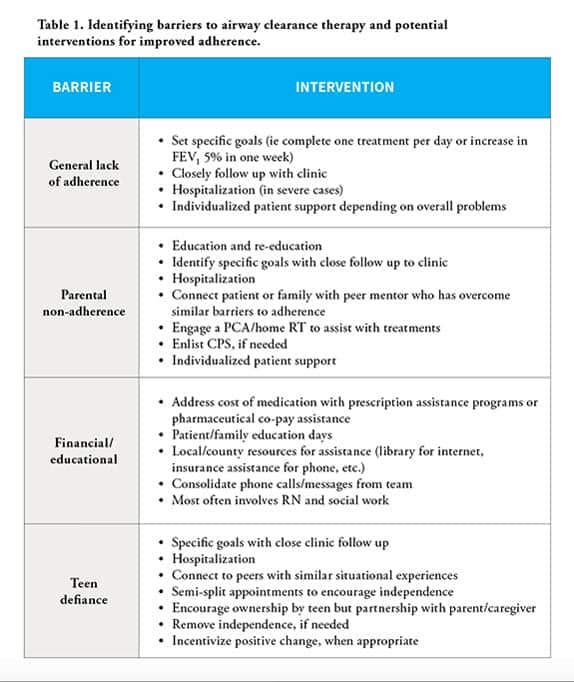
I. Identify who is at risk for non-adherence and lack of condition management.
There are various barriers to care management for pediatric patients, but some common barriers can include:
- General, overall lack of adherence. This can include a lack of compliance with medication, respiratory therapy, diet, and more.
- Parental non-adherence to therapy regimen. Parents or caregivers can often feel there is too much to get done and not enough time; or: “My kid appears to be like other kids, so why do all this work?”
- Financial barriers. Limited access to technology and devices due to financial strain, limited internet access, or limited access to transportation can all interfere with therapy adherence. Financial burdens also can be driven by multiple, expensive medications, and increasing insurance copays and deductibles.
- Teen/preteen defiance. This known developmental stage varies from patient to patient.
“We ask our patients and families to do a lot; costly medications taken multiple times each day, with many hours each day spent on prevention of changes and disease progression. It is often difficult for families to gauge the impact of these medications and therapies prior to a significant decline in lung function and quality of life,” said Amy Nelson, a Minnesota-based respiratory therapist and consultant for RespirTech. “The toughest part is to figure out how to assess for non-adherence prior to chronic, irreversible changes.”
Connected technologies can facilitate the identification process for these issues. A device like RespirTech’s inCourage Airway Clearance Therapy (a Bluetooth-enabled airway clearance vest system) will feature the capability to collect patient information and relay it to a monitoring company. For participating patients, this data could then be shared with relevant partners, such as health systems, therapists, and related care providers. Data from the device could ultimately provide an indication of whether the patient is compliant with therapy, including frequency of therapy and prescribed settings. In turn, specialists involved in each patient’s care can review the data prior to patient appointments and discuss at multidisciplinary team meetings the status of the patient and what interventions may be needed.
“As a psychologist, being able to review adherence data at each visit enhances my ability to accurately identify patient patterns and barriers to adherence and to create targeted treatment goals, including opportunities for education or re-education,” said Rebecca Johnson, PhD, ABPP, a pediatric psychologist and consultant for RespirTech who works with children and adolescents who have CF. “Most importantly, it allows me to track the effectiveness of interventions and change course, as needed. It can be very positive and motivating for patients to see their progress over time reflected in a data-driven or graphic way.”
II. Use connected technologies to manage care on an ongoing basis.
Knowing which patients are at risk can only take you so far. Caregivers and specialists need to know how to best address patients at risk for non-adherence. Typically, the process begins by asking questions of the patient and caregivers: Is the patient experiencing symptoms? Could the symptoms be attributed to not adhering to therapy? Therapy data that reflects actual device use can help identify discrepancies between what patients are saying and what clinicians see in their evaluation of the patient.
According to Nelson, “Using some of these trackable data points, we are able to preplan as a multi-disciplinary team to best help each patient. It helps going into a busy clinic day with every team member on the same page. This allows us to work with the patient and family to co-create a care plan that benefits all.”
For example, a connected device’s app could display symptoms, which along with therapy data, can provide caregivers insights into whether the patient has been following the recommended therapy regimen. When data from the connected device shows lack of adherence, clinicians and caregivers could adjust and support therapy in a timely way.
“Frequently, patients don’t struggle from just one of these identified barriers; there may be multiple facets that impact adherence. A connected system for monitoring adherence can provide visible proof that facilitates meaningful conversations with families and parents to identify what they’re struggling with and why,” said Nelson. “It’s not the be-all and end-all, but it helps us use the data we have to identify barriers in the clinic, and work together to achieve the desired results. Our goal as clinicians is to help patients succeed in living with chronic illness, and we need every tool we can get to make this a reality.”
III. Monitor the effectiveness of a connected program.
After implementing interventions for at-risk patients, clinicians and caregivers should establish metrics to determine if interventions are working and if care management is improving. This starts with identifying metrics for assessing adherence based on patient treatment and goals.
Therapists can use data from connected devices and apps to see if patients are adhering with treatment plans and if individual therapy goals are being met. Other measures of success include health care system metrics, such as readmission rates and costs to treat CF patients. Data collection can be further expanded through strategic partnerships with device or digital health companies. This would facilitate ongoing quality improvement measurements that are often cumbersome and difficult for clinicians to gather. Ultimately, this helps fill gaps in our knowledge of the care process and patient experience, and improve quality of care.
“Currently, we have little more than word of mouth to understand what our patients are doing on a day-to-day basis,” said Nelson. “But with improved technology, we will have additional data to more completely illustrate multiple aspects of the disease management journey. There are multiple areas of a patient’s life and care that could benefit from greater connectivity, giving everyone involved a more complete picture of what’s needed to best manage the condition.”
Connected solutions for better pediatric airway management
There will always be barriers to care management, no matter what the condition. But connected technologies are quickly becoming a key component to removing those barriers and positively influencing outcomes. By connecting patients, medical device companies, caregivers, and specialists, there is the potential to not only collect and share useful, personalized data, but also to open the door to better communication, patient engagement, and self-management of chronic conditions—for adult and pediatric patients alike. RT
Daniel Spors is chief commercial officer at HealthFactors and a consultant for RespirTech. Gordon Sawyer is a respiratory therapist and manager of clinical services at RespirTech. For more information, contact [email protected].