Many factors have been shown to affect 30-day COPD readmissions and some hospitals have shown success in reducing their rates.
Readmissions within 30 days for patients with chronic obstructive pulmonary disease (COPD) have been in the spotlight since the CMS began penalizing hospitals due to excessive readmissions. Many factors have been shown to affect this—and some hospitals have shown good success in reducing their readmission rates. Respiratory therapists need to continue to push for involvement in this area… it is “good fit” for RT and increases our value to the healthcare team whenever we take the lead. This article will discuss the issues related to COPD readmissions and examine the reasons why some locations are making a difference.
[maxbutton id=”1″ url=”http://info.respiratory-therapy.com/regform” text=”SUBSCRIBE TO NEWS” ]
Introduction
COPD has moved up in the rankings to now be the third leading cause of death in the US. Annual direct costs of COPD are close to $50 billion and hospital admissions for acute exacerbation of COPD (AECOPD) takes up some $13.2 billion of this cost. Some 19.6% of patients who have been hospitalized for AECOPD are readmitted within 30 days of discharge.1-2 The prevalence of COPD in the US cuts a swath down through middle of the nation along the Mississippi River valley and just beyond (see Figure 1).
Figure 1. CDC: Prevalence of COPD in the United States, 2016.19
In an effort to increase quality of care and reduce readmissions in certain diseases with high readmission rates and costs, The Centers for Medicare and Medicaid Services (CMS) initiated the Hospital Readmission Reduction Program (HRRP) in 2012 and began imposing financial penalties on hospitals that crossed the line for excessive readmissions for patients with certain targeted diseases.
The initial diseases involved with the HRRP were acute myocardial infarction, heart failure, and pneumonia. In 2014 CMS expanded the diseases that would be monitored to include COPD and total hip or total knee replacement. In 2015, CMS expanded the list again to include coronary artery bypass surgery (CABG).
Readmissions for any cause for patients in these seven categories are monitored and the penalty for excessive readmissions are penalized up to a maximum of 3%. Moreover, penalties apply across-the-board for all reimbursement dollars established under the Diagnostic-Related Group (DRG) reimbursement system.3-4 This loss in CMS reimbursement can result in a major negative impact to a hospital’s bottom line if they are operating on a narrow profit margin. According to a healthcare industry news source, CMS penalties will impact the reimbursement of 2,573 hospitals in fiscal year 2018.5 As a result of the potential penalties and loss of DRG reimbursement dollars, hospitals began projects to decrease the 30-day readmissions for these seven groups of patients.
For respiratory therapists, the CMS spotlight on COPD has increased the opportunity to play a major role in improving care, reducing readmissions, and proving our worth in the healthcare team.
Comparisons and Complexities
Issues have come up in trying to evaluate publications dealing with COPD readmissions for effectiveness. Older studies have used the International Classification of Diseases–Ninth Edition (ICD-9) while more recent studies are using the much-expanded coding system ICD-10 to find the COPD patients in the electronic medical record. Studies use the DRG code 088 for COPD and in the ICD-9 codes the codes are 491, 492, and 494.6-7 ICD-10 codes related to COPD include J40 ( Bronchitis, not specified as acute or chronic), J41 (Simple and mucopurulent chronic bronchitis), J42 (Unspecified chronic bronchitis), J43 (Emphysema), and J44 (Other chronic obstructive pulmonary disease). Although there are charts that define the links between the ICD-9 and ICD-10, having the different codes associated with the different systems can make it more difficult to interpret the impact of different strategies to reduce readmissions.1
Dealing with patients who have COPD involves comorbidities. The comparisons of differing approaches and strategies in published studies are confounded by the impact of these comorbid conditions. In addition, it has been noted that in 70% of the cases where a patient with COPD is readmitted it is the comorbidity and not COPD that is the cause of the readmission.2,8
According to the 2017 report in the Global Initiative for Obstructive Lung Disease (GOLD) publication comorbid conditions include cardiovascular disease, skeletal muscle dysfunction, metabolic syndrome, osteoporosis, depression, anxiety, and lung cancer.9 Risk factors for 30-day readmission have historically included depression, socioeconomic status, heart disease, male sex, nursing home residence, age, cor pulmonale, lower quality of life, hyponatremia, elevated PCO2, anemia, prior hospitalization, longer hospital length of stay (LOS), higher number of comorbidities, long-term oxygen therapy, worse lung function, marital status, low serum magnesium, and elevated C-reactive protein. New research has brought other risk factors for readmission into the list including obstructive sleep apnea, vertebral fractures, and electrolyte and acid/base disorders.8 In addition, issues such as low socioeconomic status, low health literacy, and substance abuse have also been mentioned as increasing the risk of readmission.1,4,10
When examining research worldwide there are also some issues related to which guidelines are being used to diagnose and manage COPD. While many practitioners are familiar with the Global Initiative for Obstructive Lung Disease (GOLD) guidelines and the most recent update from 2017, the United Kingdom uses guidelines published from the National Institute for Health and Care Excellence (NICE) which was released in 2010 and expecting to have a revision released very soon.11 These issues (coding and billing used to find and track admissions, the wide variety and impact of comorbidity, and more than one recognized set of guidelines) have resulted in many strategies working to impact readmissions with varying results.
Plans, Bundles, and Outcomes
The emphasis on reducing readmissions has prompted differing approaches to attack this problem. Several approaches utilize evidence-based programs that are not disease-specific—a point that was discussed in the national COPD Readmissions Summit of 2013. These “general” programs include the Better Outcomes through Optimizing Safe Transitions (BOOST), Project Re-Engineering Discharge (Project RED) Care Transitions Intervention, and the Transitional Care Model. These programs have common approaches including: promoting adherence to practice guidelines, medication reconciliation, encouraging patient self-management, phone calls to the patient post-discharge to assess adherence to the care plan and check on symptoms, and improving the hand-off between hospitals and ambulatory care entities. Two of the programs also involve home visits to smooth out the transition from acute care to home care. However, it is notable that these programs do not directly address the issues faced by COPD patients who have unique needs. Issues such as proper inhaler technique, use of supplemental oxygen, pulmonary rehabilitation, etc, are not addressed in these approaches.12
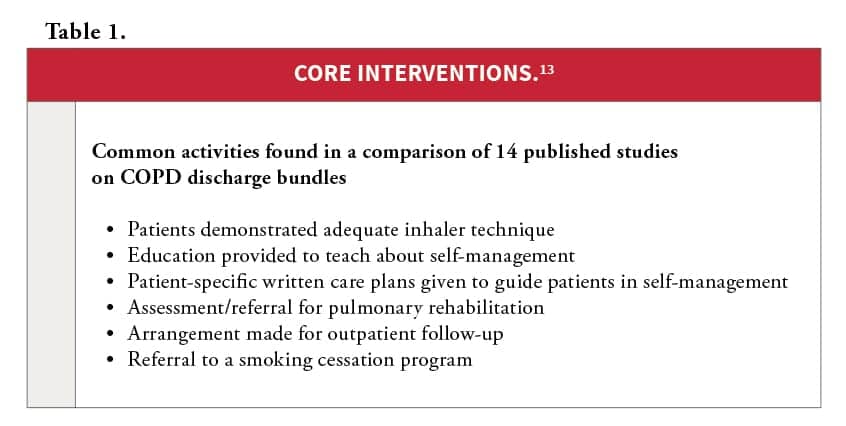
An evaluation of discharge care bundles for COPD using a meta-analysis found a broad range of interventions (from two up to 12 specific interventions) and identified 26 elements of care among all the bundles.13 The meta-analysis found 14 articles (after screening 113 potential articles for inclusion) to evaluate the effectiveness of reducing on reducing readmissions.
Across the spectrum of possible approaches, the most frequent elements of care included six activities (see Table 1). The authors state that the effectiveness of the discharge bundles on improving outcomes in the COPD population is likely multifactorial and relate to the number and characteristics of the individual elements of care and the quality with which the bundles were implemented. They concluded that consistent and reliable delivery of evidence-based care was important. They also point out that that trying to incorporate too many of the 26 elements reduced reliability and made the plans more difficult to implement. Less than half of the studies included a multidisciplinary team to implement the care bundle and the authors stated: “The diverse methodologies of studies using multidisciplinary teams for bundle implementation precluded a pooled analysis of the effectiveness on outcomes by this important implementation factor.”13
In this author’s opinion it is unfortunate that this meta-analysis was limited in the inclusion of studies using the team approach. This is a factor that needs to be examined further—a point which was made in the conclusions of this article where the authors state, “Future studies should employ higher quality research methods, fully report care bundle elements, implementation strategies and intervention fidelity to better evaluate the effectiveness of packaging evidence-based interventions together to improve outcomes of patients with COPD discharge from acute care settings.”13 The multidisciplinary team has been frequently utilized in many of the more successful bundles to plan and implement the strategies.1,6,14,15 A study published in Respiratory Care in 2017 highlighted the use of respiratory therapists functioning as disease managers with the results showing significant reduction in readmission for COPD exacerbations, length of stay, and ICU days.14
Another issue that complicates the evaluation of different strategies to uncover effectiveness lies in the time frame of the outcome. Some plans are evaluating on the impact of readmission within 30 days while others are looking at 90 days, six months, or even a year.12,16 Setting the limit at 30 days may in itself be problematic. Long-term use of the antibiotic azithromycin has been mentioned as having an impact on decreasing readmissions in the course of a year1,4 but the impact did not begin to appear until the 40-day mark.4
Various outcomes have been used to evaluate effectiveness of the strategies and this variety also complicates the process for finding the best approach. Reducing 30-day readmissions is a key, but many researchers also looked at reducing readmissions over longer periods of time (ie six to 12 months), improving quality of life, reducing length of stay (and/or reducing ICU LOS),reducing all-cause hospitalizations, reducing emergency department visits, and reducing mortality.
Factors that Influence Effectiveness of Reducing Readmission
Beyond the core interventions mentioned earlier, other factors have been explored and show some promise to influence the reduction of readmissions in COPD patients. The prevention of COPD and management of stable COPD are foundational aspects for successful care. The 2017 GOLD guidelines highlight three areas for prevention and three areas in managing stable COPD.9 The key issue in prevention is smoking cessation, followed by annual influenza vaccination and pneumococcal vaccination for all patients >65 years of age. Management of stable COPD depends on proper pharmacologic therapies (with an emphasis on proper inhaler selection and patient technique), self-management education and coaching, and routine follow-up (to monitor symptoms, exacerbations, and periodic assessment of airflow limitation in order to know when to modify the care plan and to uncover other complications and/or comorbidities that may develop.)
In the pharmacologic therapies, the guidelines mention that long-acting beta agonists (LABAs) and long-acting anticholinergics (long-acting muscarinic antagonists or LAMAs) are “preferred over short-acting agents except for patients with only occasional dyspnea.”9 Inhaled corticosteroids (ICS) are recommended for use in combination with LABAs for patients with a history of exacerbations (ICS should not be used alone as a monotherapy), and for those patients already using LABA/ICS medications who continue to have exacerbations, addition of a PDE4 inhibiter (roflumilast)1 should be considered.
GOLD mentions that all COPD patients should be screened once for the possibility that they have alpha-1 antitrypsin deficiency and if uncovered—medications addressing this should be started. GOLD also recommends that for patients with severe COPD treatment with a low-dose long acting oral and parenteral opioids may be considered to treat dyspnea. Under nonpharmacological treatments GOLD mentions instituting pulmonary rehabilitation and physical activity, nutritional supplementation, addressing end of life and palliative care, treatment of hypoxemia/hypercapnia, interventional bronchoscopy, and surgery for those who would benefit from these actions.9
Telemedicine/telehealth has been mentioned in several publications as a possible option to bring the patient improved care in the home. Video-audio links can provide education and monitor symptoms, assess general health, review inhaler technique, and allow for discussion and teaching with the benefits of both audio and visual reinforcement.1,17 Home pulse oximetry, CPAP usage, cardiac monitoring, peak expiratory flow, and portable spirometry are already in place and provide valuable information about the patient’s condition and adherence to care plans.1 A study published in 2016 looked at using telemonitoring of SpO2 and heart rate and follow-up as appropriate (by phone call, home visit, setting an office appointment, or activating a call to transport the patient to the emergency department) for values that were abnormal. Researchers found that this strategy did not have a significant effect on health-related quality of life but found that it did reduce the rate of readmission for acute exacerbation of COPD and all-cause readmissions within 30 days of discharge.18
Conclusion
Care for COPD patients to reduce 30-day readmission must include a comprehensive plan that begins in the hospital and extends into the home or patient placement in other facilities. Multiple activities rather than just one or two seem to provide the best outcomes. These activities include patient education, proper pharmacologic and nonpharmacologic interventions, a team approach for planning and implementing, and constant evaluation of effectiveness of the care bundle. Awareness of comorbidities and effective treatment of these conditions impact the readmission of COPD patients.
Factors at work outside the hospital need to be considered to ensure the patient can get their medications, can engage in activities that promote health, that they know their disease state, know their symptoms, and can follow the care plan. Many studies have shown that 30-day readmission rates can be reduced but the proper mix of interventions is still elusive. Moreover, the quality of implementing these interventions has a strong influence on success. Respiratory therapists are key players in many of the published studies and many in our profession feel that RTs have the best opportunity to champion efforts in providing a comprehensive, successful plan. RT
Bill Pruitt, MBA, RRT, CPFT, AE-C, FAARC, is a senior instructor and director of clinical education in the department of Cardiorespiratory Sciences at the University of South Alabama in Mobile. For more information, contact [email protected].
References
- Shah T, Press VG, Huisingh-Scheetz M, White SR. COPD Readmissions: Addressing COPD in the Era of Value-based Health Care. Chest 2016; 150(4):916-926.
- Rinne ST; Castaneda J; Lindenauer PK; Cleary PD; Paz HL; Gomez JL. Chronic Obstructive Pulmonary Disease Readmissions and Other Measures of Hospital Quality. Am J Resp Crit Care 2017; 196(1):47-55.
- Hoffman J, Cronin M. The true financial impact of hospital readmissions. Healthcare Financial Management. 2015; 69(1):68-76.
- Raghavan D; Bartter T; Joshi M. How to reduce hospital readmissions in chronic obstructive pulmonary disease? Curr Opin Pulm Med. 2016; 22(2):106-12.
- From Advisory.com website: https://www.advisory.com/daily-briefing/2017/08/07/hospital-penalties
- Agee J. Reducing Chronic Obstructive Pulmonary Disease 30-Day Readmissions: A Nurse-Led Evidence-Based Quality Improvement Project. Journal of Nursing Administration 2017; 47(1):35-40.
- Fidahussein S, Croghan I, Cha S, Klocke D. Posthospital follow-up visits and 30-day readmission rates in chronic obstructive pulmonary disease. Risk Manag Healthcare Policy 2014; 7: 105–112.
- Ohar JA. Risks May Not Be Reasons for COPD Readmissions. Ann Am Thorac Soc 2015; 12(9):1259-60.
- From the Global Initiative for Obstructive Lung Disease (GOLD) website. http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/
- Adamson SL; Burns J; Camp PG; Sin DD; van Eeden SF. Impact of individualized care on readmissions after a hospitalization for acute exacerbation of COPD. Int J Chronic Obstr 2016; 11:61-71.
- From the Primary Care Respiratory Society UK (PCRS-UK) website: https://pcrs-uk.org/news/update-gold-guidelines
- Krishnan JA, Gussin HA, Prieto-Centurion V, Sullivan JL, Zaidi F, Thomashow BM. Integrating COPD into patient-centered hospital readmissions reduction programs. Chronic obstructive pulmonary diseases 2015; 2(1):70-80.
- Ospina MB, Mrklas K, Deuchar L, Rowe BH, Leigh R, Bhutani M, Stickland MK. A systematic review of the effectiveness of discharge care bundles for patients with COPD. Thorax 2017; 72(1):31-39.
- Silver PC, Kollef MH, Clinkscale D, Watts P, Kidder R, et.al. A Respiratory Therapist Disease Management Program for Subjects Hospitalized With COPD. Resp Care 2017; 62(1):1-9.
- Alshabanat A, Otterstatter MC, Sin DD, Road J, Rempel C, et. al. Impact of a COPD comprehensive case management program on hospital length of stay and readmission rates. Int J Chronic Obstr 2017; 2:961-971.
- Johnson-Warrington V, Rees K, Gelder C, Morgan MD, Singh SJ. Can a supported self-management program for COPD upon hospital discharge reduce readmissions? A randomized controlled trial. Int J Chronic Obstr 2016; 11:1161-9.
- Derdak S. Prevention of COPD Readmissions: A Work in Progress. Resp Care 2017; 62(1):133-134.
- Vianello A, Fusello M, Gubian L, Rinaldo C, Dario C, et. al. Home telemonitoring for patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled trial. BMC Pulmonary Medicine. 2016; 16(1):157.
- From the CDC Behavioral Risk Factor Surveillance System https://nccd.cdc.gov/BRFSSPrevalence/ with selection for chronic health indicators–COPD. September 2017.