The use of inhaled corticosteroids for the treatment of COPD is controversial, and results of major trials are mixed.

Clinical Manifestations
The preclinical course of patients with COPD is highly variable. Patients with a history of lung disease early in life may exhibit reduced pulmonary function in adulthood. Smoking in patients with a history of childhood lung disease may lead to a progressive decline in lung function. Other patients who smoke probably begin adulthood with normal lung function. Forced expiratory volume in 1 second (FEV1) usually remains within normal limits until middle age, when a rapid decline in pulmonary function ensues. Generally, this decline stops in patients who quit smoking. The clinical symptoms of COPD usually appear in patients who continue to smoke.
Patients with COPD generally present with shortness of breath, cough, and/or wheezing. Coughing usually indicates excess mucus production. The shortness of breath is a result of increased work of breathing through obstructed airways, and is usually initially associated with increasing levels of exertion. Over time, the dyspnea worsens to the point of occurring at rest. Wheezing occurs as a result of airway narrowing, mucosal edema, and retained secretions. Classically, patients with chronic pulmonary disease have been described as either “blue bloaters” or “pink puffers.” Blue bloaters have central cyanosis with secondary polycythemia and edema. Arterial blood gas (ABG) evaluation usually reveals evidence of hypoxemia (Po2, 45-55 mm Hg), carbon dioxide retention (Pco2, 50-60 mm Hg), and compensated respiratory acidosis (pH, 7.38-7.42).7 Pink puffers do not have secondary polycythemia, and edema is not present. They have less hypoxemia (Po2, 60-80 mm Hg) and no carbon dioxide retention (Pco2, 30-40 mm Hg).7 Many patients have features of both conditions.
General Principles of Management
There are four general principles of management of the patient with COPD: (1) slow disease progression; (2) prevent infection; (3) treat reversible symptoms; and (4) educate patients. The respiratory care practitioner is intimately involved in all four cornerstones of care.
Slow Disease Progression
If the extent of disease is not completely irreversible (end-stage), progression of disease can be slowed by smoking cessation, reduction of exposure to environmental or occupational irritants, and therapy with supplemental oxygen.
Prevent Infection
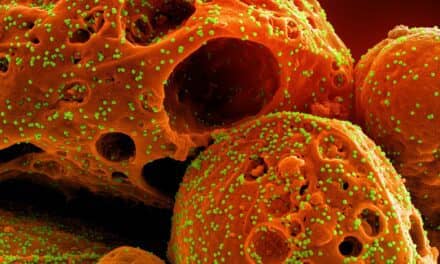
Infection is usually considered the main cause of acute exacerbation in COPD, although many COPD patients have evidence of lower respiratory tract bacterial colonization even during periods of remission.8 In fact, potentially pathogenic organisms can be recovered from the respiratory tract secretions of virtually all patients with COPD at some time during the course of their disease.8 Many bacterial and other organisms have been found in the sputum of patients with chronic pulmonary disease. These include Haemophilus influenzae; Streptococcus pneumoniae; Streptococcus viridans; Klebsiella species; Moraxella (formerly called Branhamella) catarrhalis; Staphylococcus aureus; Staphylococcus epidermidis; and Candida albicans (a fungus). Nonetheless, the role of antibiotic therapy in acute exacerbations of COPD remains controversial. Broad-spectrum antibiotic prophylaxis has not been shown to decrease the frequency of infections, but may decrease the severity and duration of symptoms. Recent evidence has shown that bacterial colonization is associated with enhanced airway inflammation and that resolution of bronchial inflammation following acute exacerbations of chronic bronchitis may be related to bacterial eradication.9
Patients with COPD should be encouraged to have annual influenza vaccinations. Some authorities also recommend vaccination against pneumococcal disease.
Treat Reversible Symptoms
Pharmacotherapy with inhaled ß2-agonists and long-acting theophylline preparations may reverse the symptoms of airway obstruction. The use of inhaled corticosteroids (ICS) is reviewed later in this article.
Educate Patients
Education should be an integral part of chronic pulmonary disease management. Patients and their families should be given basic facts about the disease process and offered a list of resources in the event they desire additional information. Medication issues should be addressed. If appropriate, the subject of intubation and resuscitative intervention should be reviewed and the patient’s desires should be delineated.
Surgery
Surgical procedures for COPD are very rare. They are expensive and often not covered by insurance. The great majority of patients cannot be helped by surgery, and no single procedure is ideal for those who can be helped.
Lung transplantation has been successfully employed in some patients with end-stage COPD. After transplantation, pulmonary function is usually markedly improved. Postoperatively, dyspnea at rest is abolished in most patients, and dyspnea on exertion is significantly diminished. Supplemental oxygen is usually no longer required, and exercise tolerance is markedly improved. Unfortunately, lung transplantation is associated with potentially severe complications, including pulmonary edema, ventilation-perfusion abnormalities, and organ rejection. In the hands of an experienced team, the 3-year survival rate is approximately 50%.10,11
Lung volume reduction surgery (LVRS) removes 20% to 30% of severely diseased lung tissue; the remaining parts of the lung are joined together. Mortality rates can be as high as 15% and complication rates are even higher. When the operation is successful, patients report significant improvement in symptoms.12
Pulmonary Rehabilitation
A structured, outpatient pulmonary rehabilitation program improves functional capacity in certain patients with COPD. Services may include general exercise training, administration of oxygen and nutritional supplements, intermittent mechanical ventilatory support, continuous positive airway pressure (CPAP), relaxation techniques, breathing exercises and techniques (such as pursed lip breathing), and methods for mobilizing and removing secretions.
Use of Inhaled Corticosteroids
ICS are used for long-term maintenance treatment in COPD, but the efficacy of these agents is controversial.
There are at least two possible reasons why COPD patients might respond to anti-inflammatory treatment, despite the general acknowledgment that the loss of lung tissue elasticity is relatively fixed. Some asthma patients may be misdiagnosed as COPD. The differentiation of severe COPD from chronic severe asthma can be difficult because some degree of reversibility (shown as improvement in FEV1) can be achieved in the majority of patients.13 The pathological changes of bronchial asthma in the large airways can coexist with those of COPD, which predominantly affects the small airways. Patients with COPD who respond to corticosteroids may have a degree of inflammation, which may be component specific to the disease.
While the presence of inflammatory changes in the airways of patients with COPD14 provides a rationale for the use of corticosteroids, the association between these changes, lung function, and the therapeutic response to corticosteroids has not yet been established clearly. Several uncontrolled retrospective studies performed in the 1980s suggested that long-term treatment with oral corticosteroids might slow the decline in FEV1 in patients with COPD.15,16 Long-term use of oral corticosteroids would not generally be recommended because of the risk of systemic adverse events, however. Inhaled corticosteroids offer an option for achieving similar benefits with fewer systemic side effects. More recent investigations evaluating the efficacy of corticosteroids in COPD have focused on inhaled agents.
Trials Have Mixed Outcomes
An early trial of ICS in COPD suggested an improvement in FEV1 and reduction in the decline in FEV1 over 1 year of treatment with inhaled beclomethasone.17 A 2-year study with inhaled budesonide (1,600 µg/day) showed significant reduction in respiratory symptoms,18 with a halving of the median decline in FEV1 in a group of nonallergic patients with COPD (30 mL/year in the budesonide group, compared to 60 mL/year in the placebo group). The number of patients withdrawing due to pulmonary problems was significantly higher in the placebo group.
The ISOLDE (Inhaled Steroids in Obstructive Lung Disease in Europe) study was a UK-based, multicenter, double-blind, placebo-controlled study of fluticasone (500 µg twice daily) in 753 patients with moderate-to-severe COPD, with the main outcome measure being the rate of decline of postbronchodilator FEV1 over 3 years.19 Secondary endpoints were the frequencies of exacerbations, changes in health status, withdrawals because of respiratory disease, morning serum cortisol concentrations, and adverse events. Patients recruited had a diagnosis of COPD, were aged 40 to 75 years, and had a postbronchodilator ratio of FEV1 to FVC less than 70%. The average prebronchodilator FEV1 was 1.24 L, suggesting that the participants had severe COPD. There was no difference in the decline of respiratory function, as measured by FEV1, over the 3 years of the study in the fluticasone or placebo groups (59 mL/year versus 50 mL/year). The yearly exacerbation rate was lower in the fluticasone group than in the placebo group (0.99 versus 1.32 per year; P=0.026). Health status, measured by the increase in questionnaire score, declined at a slower rate in the fluticasone group than in the placebo group (2.0 versus 3.2 units/year; P=0.004). Adverse effects were similar in each group. The only clinical benefit seen in this trial was a decrease in the frequency of exacerbations requiring oral steroid or antibiotic treatment.
The EUROSCOP (European Respiratory Society Study on Chronic Obstructive Pulmonary Disease) study compared budesonide 400 µg bid, to placebo in actively smoking subjects with mild COPD (mean FEV1, 2.54 L) over a period of 3 years.20 The primary outcome was the rate of postbronchodilator decline in the FEV1. Over the first 6 months of the study, the FEV1 improved by about 10 mL in the budesonide group while it declined by about 40 mL in the placebo group. Thereafter, the rates of FEV1 decline were nearly similar in the two treatment groups. Patients receiving active treatment experienced significantly more skin bruising and adverse upper airway effects. Thus, relatively large doses of ICS given for 3 years to smokers with mild COPD were associated with some side effects and limited benefit.
A meta-analysis of five randomized, placebo-controlled trials of ICS in patients with COPD was performed to evaluate the long-term effects of these agents on the rate of FEV1 decline in patients with COPD.21 The use of ICS did not change the rate of FEV1 decline in 3,571 patients followed for 24 to 54 months.
Investigators have evaluated, in a randomized, double-blind, parallel-group, placebo-controlled study, whether the combination of inhaled ß2-agonists and ICS provides better pulmonary outcomes than treatment with either agent alone in patients with COPD.22 Subjects were treated with either salmeterol 50 µg bid (n=372), fluticasone 500 mg bid (n=374), the combination of both (n=358), or placebo (n=361) for 12 months. All of the active treatments improved lung function, pulmonary symptoms, and health status and reduced use of rescue medication and frequency of exacerbations. Combination therapy improved pretreatment FEV1 significantly better than did placebo, salmeterol alone, or fluticasone alone. Combination treatment also produced a clinically significant improvement in health status and the greatest reduction in daily symptoms. Based on these results, the investigators suggested that the combination of inhaled long-acting ß2-agonists and corticosteroids be considered for patients with COPD.
Since the ISOLDE results19 were published, a number of investigators have reported improvements in health-related quality of life in patients with moderate to advanced COPD treated with inhaled corticosteroids.23-25 The Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines recommend a trial of inhaled corticosteroids for patients with an FEV1 <50% of predicted and a clinical course characterized by significant symptoms or repeated exacerbations.26,27
Summary
The evidence base supporting efficacy for ICS in COPD is growing, but the results of major trials are still mixed, and the use of ICS in COPD is still considered controversial. The therapy of COPD should be tailored to the individual patient. The GOLD guidelines suggest using ICS in selected patients with moderate to severe disease.26,27 Some clinicians suggest targeting use of ICS to those patients who respond to a 2-week trial of these agents.
John D. Zoidis, MD, is a contributing writer for RT.
References
1. Ferguson GT, Cherniack RM. Management of chronic obstructive pulmonary disease. New Engl J Med. 1993;328:1017-1022.
2. Halbert RJ, Isonaka S, George D, Iqbal A. Interpreting COPD prevalence estimates: what is the true burden of disease? Chest. 2003;123:1684-1692.
3. Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest. 2002;121(suppl):121S-126S.
4. Stang P, Lydick E, Silberman C, Kempel A, Keating ET. The prevalence of COPD: using smoking rates to estimate disease frequency in the general population. Chest. 2000;117(suppl):354S-359S.
5. Petty TL. Definition, epidemiology, course, and prognosis of COPD. Clin Cornerstone. 2003;5:1-10.
6. Thurlbeck WM. Pathophysiology of chronic obstructive pulmonary disease. Clin Chest Med. 1990;11:389-403.
7. Celli BR, MacNee W. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932-946.
8. Fagon JY, Chastre J. Severe exacerbations of COPD patients: the role of pulmonary infections. Semin Respir Infect. 1996;11:109-118.
9. White AJ, Gompertz S, Bayley DL, et al. Resolution of bronchial inflammation is related to bacterial eradication following treatment of exacerbations of chronic bronchitis. Thorax. 2003;58:680-685.
10. Trulock EP 3rd. Lung transplantation for COPD. Chest. 1998;113(suppl):269S-276S.
11. Hosenpud JD, Novick RJ, Bennett LE, Keck BM, Fiol B, Daily OP. The Registry of the International Society for Heart and Lung Transplantation: thirteenth official report—1996. J Heart Lung Transpl. 1996;15:655-674.
12. Meyers BF, Patterson GA. Chronic obstructive pulmonary disease. 10: Bullectomy, lung volume reduction surgery, and transplantation for patients with chronic obstructive pulmonary disease. Thorax. 2003;58:634-638.
13. British Thoracic Society. Guidelines for the management of chronic obstructive pulmonary disease. Thorax. 1997;52:S1-S32.
14. Donaldson GC, Seemungal TA, Patel IS, et al. Airway and systemic inflammation and decline in lung function in patients with COPD. Chest. 2005;128:1995-2004.
15. Postma DS, Peters I, Steenhuis EJ, et al. Severe chronic airflow obstruction: can corticosteroids slow down progression? Eur J Respir Dis. 1985;67:56-64.
16. Postma DS, Peters I, Steenhuis EJ, et al. Moderately severe chronic airflow obstruction. Can corticosteroids slow down progression? Eur Respir J. 1988;1:22-26.
17. Dompeling E, van Schayck EP, Molema J, et al. Inhaled beclomethasone improves the course of asthma and COPD. Eur Respir J. 1992;5:945-952.
18. Renkema TE, Schouten JP, Koeter GH, et al. Effects of long-term treatment with corticosteroids in COPD. Chest. 1996;109:1156-1162.
19. Burge PS, Calverly PM, Jones PW, Spencer S, Anderson JA, Maslen TK. Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trial. Br Med J. 2000;320:1297-1303.
20. Pauwels RA, Lofdahl C-G, Laitinen LA, et al. Long-term treatment with inhaled budesonide in persons with mild chronic obstructive pulmonary disease who continue smoking. N Engl J Med. 1999;340:1948-1953.
21. Highland KB, Strange C, Heffner JE. Long-term effects of inhaled corticosteroids on FEV1 in patients with chronic obstructive pulmonary disease. A meta-analysis. Ann Intern Med. 2003;138:969-973.
22. Calverley P, Pauwels R, Vestbo J, et al. Combined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomised controlled trial. Lancet. 2003;361:449-456.
23.van den Boom G, Rutten-van Molken MP, Molema J, Tirimanna PR, van Weel C, van Schayck CP. The cost effectiveness of early treatment with fluticasone propionate 250 microg twice a day in subjects with obstructive airway disease. Results of the DIMCA program. Am J Respir Crit Care Med. 2001;164:2057-2066.
24. Thompson WH, Carvalho P, Souza JP, Charan NB. Controlled trial of inhaled fluticasone propionate in moderate to severe COPD. Lung. 2002;180:191-201.
25. van der Valk P, Monninkhof E, van der Palen J, Zielhuis G, van Herwaarden C. Effect of discontinuation of inhaled corticosteroids in patients with chronic obstructive pulmonary disease: the COPE study. Am J Respir Crit Care Med. 2002;166:1358-1363.
26. Fabbri LM, Hurd SS. Global strategy for the diagnosis, management and prevention of COPD: 2003 update. Eur Respir J. 2003;22:1-2.
27. Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med. 2001;163:1256-1276.