A federal judge ruled that Congress, not CMS officials, should set Medicare payment rates. An article this week from Robert Pear of the New York Times highlighted the decision which effectively blocked the Bush Administration’s effort to save money on Medicare by paying for only the least expensive treatments for particular conditions, primarily COPD.
Decided in mid October, the case is just now receiving attention from Medicare officials and media. “Congress sets Medicare payment rates and never intended to give officials broad discretion to alter them, the court said in an important test case on Oct. 16,” wrote Pear in the NY Times. “Judge Henry H. Kennedy Jr. of Federal District Court here said the policy of paying for only ‘the least costly alternative’ was not permitted under the Medicare law.”
Kennedy says the administration’s position would lead to “enormous discretion” on the part of the HHS secretary to determine amounts paid for Medicare, with little regard for the detailed pricing formulas set by Congress. Ultimately, Kennedy wrote that this “flies in the face of the detailed statutory provisions.”
“Over the years, Medicare officials have often tried to adopt regulations that allow them to consider cost in deciding whether the program should cover various goods and services,” writes Pear. “Health care providers, manufacturers and some patients’ advocates have resisted these efforts, saying that coverage decisions should be made based on clinical effectiveness and not cost.”
The Times quotes a CMS spokesman who disagrees with the ruling, saying that officials are still considering further legal steps. Unnamed Federal health officials contend that the decision will make it more difficult to rein in spiraling Medicare costs.
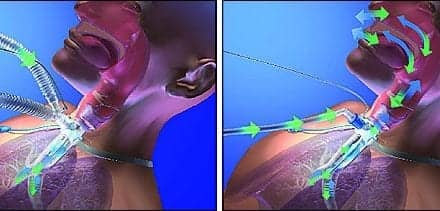
Specifically, Judge Kennedy ruled that CMS and some of its contractors had unlawfully limited payments for DuoNeb, an inhalation drug taken through a nebulizer. One dose provides a combination of two commonly prescribed bronchodilators, albuterol and ipratropium. Click here to read the full NY Times article.