Biodesix has presented positive data for a blood-based test with the potential to detect a non-small cell lung cancer (NSCLC) patient’s pre-treatment risk of anti-PD-1 immunotherapy resistance.
[maxbutton id=”1″ url=”http://info.respiratory-therapy.com/regform” text=”SUBSCRIBE TO NEWS” ]
Biodesix’s primary immunotherapy resistance test demonstrated utility in classifying NSCLC patients treated with nivolumab by overall survival. The test classification is independent of PD-L1 status.
“Anti-PD-1 therapy is capable of restoring immunity and has greatly increased overall survival rates for patients. However, we know that this therapy does not benefit everyone,” said lead author Egbert Smit, MD, PhD, of the Netherlands Cancer Institute, Department of Thoracic Oncology in Amsterdam. “A test that can determine which patients will respond poorly to immunotherapy, would greatly optimize treatment regimens.”
Immune checkpoint inhibitors have disrupted traditional cancer treatment and increased overall survival rates for many patients. Hyperprogressive disease (HPD) is a new and disastrous pattern of progression in some cancer patients treated with anti-PD-1/PD-L1 therapy. A recent study published in JAMA Oncology found that HPD is more common in advanced NSCLC patients treated with anti-PD-1/PD-L1 inhibitors, as compared to patients treated with chemotherapy.
“These data show us that a liquid biopsy test for primary immunotherapy resistance could identify patients likely or unlikely to benefit from monotherapy,” said David Brunel, CEO for Biodesix. “We are working toward validating this test in a prospective study. Evaluation in front-line treatment with immuno-oncology combinations is already in progress.”
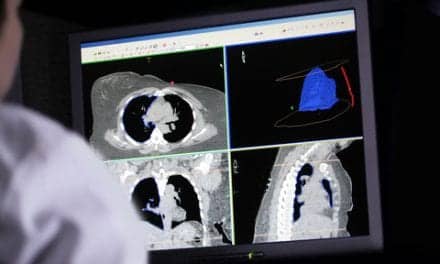
The Biodesix primary immunotherapy resistance test uses Deep Maldi mass spectrometry to probe the circulating proteome in blood. The immunotherapy resistant subgroup in the test demonstrated increased activation in the complement, acute phase, extra-cellular matrix and wound healing biological pathways.