Objective
To describe the successful clinical management of a patient with acute respiratory distress syndrome (ARDS) using airway pressure release ventilation (APRV).
Case Summary
A 19-year-old patient complained of a severe headache and collapsed in front of his parents and became unresponsive. He was intubated at the scene and then taken by paramedics to the emergency department where he was found to have a large intracranial hemorrhage involving left parietal-occipital lobes with edema, shift, and herniation. However, approximately four hours after arriving from the outside facility, the patient began desaturating and required 100% FiO2 to maintain oxygenation saturations in the 90s. His PEEP was increased up to 15 cm H2O and tidal volumes maintained at 6 cc/kg, but he continued to desaturate into the low 80s on 100% FiO2.
A chest radiograph showed bilateral alveolar opacification, believed to be a combination of neurogenic pulmonary edema and possible acute respiratory distress syndrome (ARDS). After placing him on nitric oxide, the patient showed no signs of improvement. During the initial placement of APRV, the patient experienced a brief episode of desaturation. However, oxygen saturations stabilized and increased into the 90s. During the initial hours of APRV, the patient was spontaneously breathing and did not show any signs of agitation or discomfort. The patient’s oxygenation continued to improve and the patient was weaned back to pressure controlled ventilation PCV.
New or Unique Information Provided
The use of APRV in a patient with intracranial hemorrhage can be successfully implemented to treat ARDS. APRV is usually contraindicated with intracranial hemorrhages. However, APRV can be considered a feasible alternative.
Keywords
Airway Pressure Release Ventilation (APRV), Time High (THigh), Time Low (TLow), Pressure High (PHigh), Pressure Low (PLow), Cerebral Perfusion Pressure (CPP)
Introduction
Airway pressure release ventilation (APRV) is inverse ratio, pressure controlled, intermittent mandatory ventilation with unrestricted spontaneous breathing.1 APRV is a unique method of providing ventilator support by using a bilevel positive airway pressure model with most of the respiratory cycle spent at the high pressure with intermittent release ventilations. This method allows the patient to have higher mean airway pressures at lower high pressures and can lead to improvement in oxygenation and use less sedation and no paralysis. Another advantage over other rescue therapies, like high frequency oscillatory ventilation (HFOV), is that patients are spontaneously breathing and can cough to clear secretions.
Historically, clinicians have been reluctant to use APRV in patients with traumatic brain injury (TBI) due to higher mean airway pressure impeding cerebral venous return and less reliable ventilation causing elevated pCO2 and potentially increasing intracranial pressures (ICP).2 We present a case where APRV was utilized in order to facilitate serial neurologic exams in a patient with severe TBI.
Case Summary
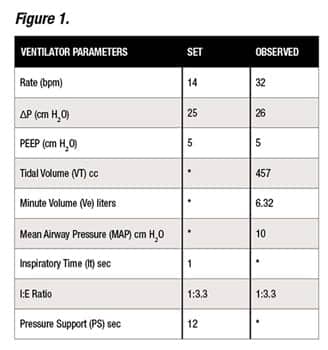
A 19-year-old patient that complained of a severe headache and collapsed in front of his parents and became unresponsive. He was intubated at the scene and then taken by paramedics to the emergency department where he was found to have a large intracranial hemorrhage involving left parietal-occipital lobes with edema, shift and herniation. The patient had an emergent left parietal craniotomy with evacuation of the hematoma and was transferred to a pediatric intensive care unit for further management. The patient was initially placed on Pressure Control/Pressure Support (PC/PS) ventilation. (See Figure 1.)
Patient Weight: 75 kg and receiving 3% Saline IV; Blood Pressure: 136/71; ICP: 16 cm H2O; and CPP: 70 cm H2O. Patient had an arterial line in place.
Initial arterial blood gas (ABG) on 50% FiO2: (See Figure 2)
His initial PO2/ FiO2 ratio was 254. However, approximately four hours after arriving from the outside facility, the patient began desaturating and required 100% FiO2 to maintain oxygenation saturations in the 90s. His PEEP was increased up to 15 cm H2O and tidal volumes maintained at 6 cc/kg, but he continued to desaturate into the low 80s on 100% FiO2.
Recruitment maneuvers were attempted utilizing hand ventilation for five minutes without any improvement. A chest radiograph showed bilateral alveolar opacification felt to be a combination of neurogenic pulmonary edema and possible acute respiratory distress syndrome.
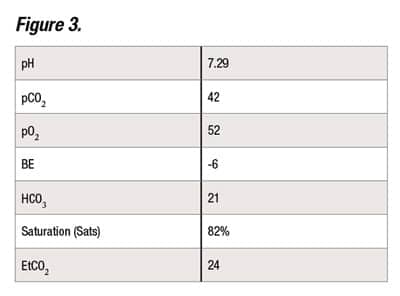
An ABG was drawn. (See Figure 3.)
The patient was placed on inhaled nitric oxide (iNO) therapy at 20 parts per million (ppm), but there was no improvement oxygenation. High frequency oscillatory ventilation (HFOV) was considered, but both the need for paralysis obscuring the neurological exam and high MAP impeding cerebral venous return were felt to be contraindications. For those reasons, APRV appeared to be a better alternative.
The goals of APRV were to: be able to assess neurological status, improve oxygenation, and reduce or reverse pulmonary edema, while not needing the use of neurological paralytic agents such as Vecuronium.
During the initial placement of APRV, the patient experienced a brief episode of desaturation. However, oxygen saturations stabilized and increased into the 90s. During the initial hours of APRV, the patient was spontaneously breathing and did not show any signs of agitation or discomfort. Fentanyl was maintained at 1 mcg/kg/hr and there was no increase in ICP. (See Figure 4.) Over the next two days, the patient’s oxygenation continued to improve and the patient was weaned back to PC/PS. (See Figure 5.)
Discussion
Elevated intrathoracic pressure can lead to impaired cerebral venous return and, consequently, elevated intracranial pressure. For this reason, many clinicians have not employed HFOV or APRV in patients with severe head injury.
Our patient’s lung disease made it impossible to achieve adequate oxygenation despite maximizing the settings on conventional ventilation. We were able to successfully transition the patient over to APRV while maintaining the ability to assess his underlying neurological exam.
During the two days on APRV, oxygenation continued to improve and intracranial pressure remained stable. We did not encounter any elevation of the ICP or reduction of CPP despite using an initial MAP over 30 cm H2O. Despite concerns of potential inadequate ventilation from APRV, we were able to maintain normal pCO2 throughout the course.
By utilizing APRV, we were able to oxygenate and ventilate the patient adequately while the underlying neurologic pulmonary edema had a chance to improve. APRV should be considered for patients with severe head injury that encounter problems with oxygenation. RT
Gus Matamoros, RRT, RCP, NPT, NPS, and Jennifer Czaplicki, RRT, RCP work in the department of Respiratory Care at Miller Children’s Hospital, Long Beach, Calif. For this article, Matamoros wrote the case presentation, obtained the clinical data, and cared for the patient in the PICU. Meanwhile, Czaplicki obtained the clinical data, cared for the patient, and assisted with writing the case presentation. Neither author reports any conflict of interest with this paper. For more information contact [email protected].
Acknowledgements
The authors would like to thank Mark Grzeskowiak, RCP, Glenn Levine, MD, and Christopher Babbitt, MD, for their valuable help and constructive criticism with this case presentation.
References
-
Daoud, Ehab G; Farag, Hany L; Chatburn, Robert L. “Airway Pressure Release Ventilation: What do We Know?” Respiratory Care. Feb 2012. 57:2:282-292 (11)
-
Davis, Brandy L.; Saunders, Peter; et al. “Use of Airway Pressure Release Ventilation with Traumatic Brain Injured Patient Respiratory Care.” Respiratory Care. Accessed from: www.rcjournal.com/abstracts/2011