Spirometry is only part of complete pulmonary function testing, but even as a stand-alone test, it can provide valuable information.
By Lawrence Martin, MD
Editor’s note: Click here for Part 2, where Dr Martin discusses the use of spirometry in gauging severity of impairment, and for following serial changes in lung function. Some figures/diagrams no longer available.
I consider spirometry one of the fundamental tests in clinical medicine, like the ECG, chest x-ray, electrolytes, pulse oximetry, and complete blood count (CBC). Spirometry is different from other basic tests in one important aspect: effort dependency. The patient must give maximum expiratory effort in a coordinated fashion, and good results require coaching from a skilled and enthusiastic pulmonary function technician. The necessity of coordinated effort has made spirometry less popular than most other basic tests (it has no utility if the patient can’t cooperate), but nonetheless invaluable in the right setting.
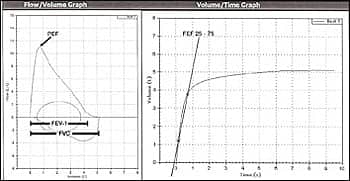
Figure 1. Spirometry requires the subject to inhale maximally, blow all the air out forcefully through a large bore tube, and then inhale rapidly and fully; the expiratory effort normally takes 4 to 6 seconds. The spirometer measures airflow and volume exhaled. The test can be displayed graphically, as either a flow-volume loop (left) or a time-volume plot (right). In the flow-volume loop, exhalation is above the horizontal axis, inhalation below. (The oval circle is a regular breath.) Specific values for forced vital capacity (FVC), forced expiratory volume in 1 second (FEV1), ratio of FEV1/FVC, peak expiratory flow (PEF), and forced expiratory flow between 25% and 75% of FVC (FEF 25-75) can be reported, along with an interpretation. On the flow-volume loop, PEF is read on the vertical axis for flow rate, and FEV1 and FVC on the horizontal axis for lung volume in liters. FEF 25-75 is the slope of a line drawn between 25% and 75% of the FVC on the time-volume plot. Values from this normal spirometry are shown below. Traditionally, FVC, FEV1, FEV1/FVC, and FEF 25-75 are reported as a percent of predicted, with normal +/- 20% of that value. The ratio FEV1/FVC is reported as a percent absolute; the predicted value is considered the minimum, with anything lower indicating some degree of airflow obstruction. |
Spirometry is one part of complete pulmonary function testing, which also includes measurement of total lung capacity (TLC) and its components, and diffusion capacity. However, spirometry as a stand-alone test can give much useful information. A review of spirometry is outside the scope of this article, and I will not discuss standards for testing, patterns of impairment (restriction, lower and upper airway obstruction, etc), or airway challenge tests. These and other aspects are discussed in numerous articles and texts.1-3 Instead, I will focus on four principal uses of spirometry in the daily practice of pulmonary medicine:
- To help in diagnosis of patients who complain of dyspnea or chronic cough;
- To differentiate between asthma and chronic obstructive pulmonary disease (COPD), and help guide treatment;
- To gauge severity of impairment for both clinical and disability evaluations; and
- To follow serial changes in lung function when clinically warranted.
Help in Diagnosis of Patients Who Complain of Dyspnea or Chronic Cough
What is the most common cause of chronic cough (>3 weeks’ duration)?
- Asthma
- Chronic obstructive pulmonary disease (COPD)
- Rhinitis/post-nasal drip
- ACE inhibitor therapy for hypertension
Both dyspnea and chronic cough are common problems in clinical practice. While it is widely taught that asthma can present as chronic cough (>3 weeks’ duration) without wheezing, this is uncommon. By far, the most common cause of chronic cough is rhinitis/post-nasal drip. Nonetheless, when a cause of chronic cough is not evident from the history and physical exam, spirometry may be indicated to look for airflow obstruction and reversibility with an inhaled bronchodilator—hallmarks of asthma. Patients with unexplained dyspnea also warrant spirometry testing. If spirometry is normal, the patient’s dyspnea is likely not from pulmonary impairment. Conversely, if the test is abnormal, then pulmonary impairment may be the cause. (Note that if the physician strongly suspects asthma in a patient with normal spirometry, a methacholine challenge test, MCT, may be ordered. Essentially, the MCT is a series of spirometries after graded inhalations of methacholine.3 A fall in FEV1 by more than 20% from baseline indicates airway hyperreactivity and a possible diagnosis of asthma, even though baseline spirometry is normal.)
Case 1 (Mr L)
 |  |
| Figure 2. Normal spirometry. Spirometry is normal: FVC = 4.31 L (106% predicted), FEV1 = 3.70 L (108% predicted), FEV1/FVC = 86% absolute. | Figure 3. Severe flow obstruction. Pre-bronchodilator spirometry shows severe airflow obstruction (blue loop), with minimal bronchodilator response (red loop). Pre-bronchodilator values: FVC = 1.71 L (59% predicted), FEV1 = 0.86 (36% predicted), FEV1/FVC = 50% absolute. |
Mr L, age 46, was seen in consultation for history of “trouble breathing.” The symptom of dyspnea had been present for 2 months, and necessitated one emergency department visit 2 months earlier. Chest x-ray at that time was normal, and he was treated with a bronchodilator and sent home. He has a 15-pack-year smoking history, but there is no confirmed diagnosis of COPD or asthma. He manages a used car dealership, a job that causes “a lot of stress.” He complains of frequent inability to take a deep breath and states, “Sometimes I feel shortness of breath when climbing stairs.” He takes no medications. Evaluations prior to his pulmonary consultation included cardiac stress test and CBC (both normal). He is 67 inches tall, and weighs 220 pounds. Lungs were clear on auscultation. He has a crowded posterior pharynx, but the rest of the exam was unremarkable. Further history reveals recent onset of choking sensations that awaken him at night, and his wife has said he snores heavily. Spirometry was normal (Figure 2). In this case, spirometry was useful in ruling out any airways obstruction. When combined with the normal chest x-ray and lung exam, it became apparent he has no pulmonary cause for dyspnea. An overnight polysomnogram revealed obstructive sleep apnea, which was treated with CPAP. His dyspnea symptom was attributed to anxiety over nocturnal awakenings, plus some physical conditioning. With nightly CPAP, he feels significantly better.
Case 2 (Ms J)
Ms J, age 57, was admitted to hospital for new onset congestive heart failure (CHF). She had a 40-pack-year smoking history but no prior diagnosis of lung disease. Chest x-ray on admission showed cardiomegaly and changes of congestive heart failure. She improved with medical management and after discharge was followed by her cardiologist. Chest x-ray 1 month later showed near normal heart size and clear lung fields, but she continued to complain of dyspnea on exertion. Medications were adjusted, and 2 months later an echocardiogram showed low normal ejection fraction. Dyspnea on exertion continued, and she was referred for pulmonary evaluation. On exam, her lungs were clear to auscultation. Spirometry showed severe airflow obstruction (Figure 3), heretofore undiagnosed. She admitted to long-standing dyspnea on exertion, made worse by the episode of CHF. Although cardiac function improved, dyspnea remained a prominent symptom and was attributed to poor lung function. She was treated with tiotropium inhaler and entered a pulmonary rehab program. In this case, spirometry clarified the cause of her dyspnea, and made further cardiac evaluation unnecessary.
Differentiating Between Asthma and COPD
What is the principal clinical difference between asthma and COPD?
- Types and doses of drugs used for treatment
- Degree of expected improvement in spirometry
- Smoking history
- Patient symptoms by numerical scoring criteria
There can be much confusion over whether a patient with dyspnea and wheezing has COPD or asthma. In clinical practice, there is one principal distinction: degree of improvement in airflow. Irrespective of smoking history, the diagnosis is COPD if airflow obstruction does not normalize or come close to normal with maximum treatment. If spirometry returns to normal or near normal with maximum treatment, the diagnosis is asthma (or asthmatic bronchitis) and not COPD. A corollary is that spirometry, while not essential for treatment, is essential for proper diagnosis of either condition.
One of the causes of COPD is untreated or undertreated asthma, so when a patient presents with wheezing, it is important to maximize treatment in attempt to fully reverse airflow obstruction. Patients presenting with wheezing in whom the question arises—COPD or asthma?—should be given oral corticosteroids and bronchodilator therapy for a short period (1-2 weeks), and followed up with repeat spirometry.
 |  |
| Figure 4a. | Figure 4b. |
Spirometry is abnormal in February (4a), with pre-bronchodilator (blue curve) FVC = 54% predicted, FEV1 = 41% predicted. In April (4b), after 1 week of prednisone, spirometry is normal (FVC = 105% predicted, FEV1 = 99% predicted).
Case 3 (Ms P)
Ms P, age 60, developed cough and dyspnea on exertion in late December. She is a nonsmoker with a history of “seasonal allergies.” She was initially treated with antibiotics; when symptoms persisted into January, she received a course of prednisone, which made her feel better. As soon as the drug was stopped, her cough and wheezing resumed. A pulmonary function test in mid-February showed severe airflow obstruction with a brisk bronchodilator response (Figure 4a). She was treated again with prednisone and symptoms improved somewhat, only to recur when the medication was stopped. She was referred for pulmonary consultation, and on exam March 30 (almost 4 months after initial symptoms) she had wheezing on auscultation.
As is typical of patients with chronic airflow obstruction, she was in no distress at rest and did not use accessory breathing muscles. She was immediately started on high dose prednisone, and asked to continue inhaled bronchodilator. She returned in early April, feeling considerably improved. Wheezing was gone and spirometry was normal (Figure 4b). By slowly tapering prednisone over the following 3 weeks, she maintained normal airway function. Without spirometry as a guide, she might have remained chronically under-treated.
RT
Lawrence Martin, MD, is board-certified in pulmonary and sleep medicine. He is clinical professor of medicine, Case Western Reserve University School of Medicine, Cleveland. For further information, contact [email protected].
Editor's note: Click here for Part 2, where Dr Martin discusses the use of spirometry in gauging severity of impairment, and for following serial changes in lung function.
| What About Screening Spirometry? Screening spirometry refers to testing a set of people who meet specific, pre-established criteria, such as workers exposed to chemicals like diacetyl or benzene, or dusts such as coal and silica. In 2000 the National Lung Health Education Program (NLHEP) recommended that all smokers >45 years old have screening spirometry to identify undiagnosed COPD.4 This recommendation led many physicians to establish office spirometry and treat patients when COPD was discovered. In 2008 this recommendation was rescinded after an extensive review by the Agency for Healthcare Research and Quality (AHRQ) found screening spirometry not to be beneficial.5,6 The AHRQ report found that “Widespread spirometric testing is likely to label a large number of individuals (many who do not report respiratory symptoms) with disease and result in considerable testing and treatment costs and health-care resource utilization.”5 The evidence also did not show that screening spirometry led to more smoking cessation than drug therapy (eg, nicotine replacement) or physician counseling.7 Occupation-based screening spirometry remains widely practiced, both to determine fitness for work in certain areas (primary prevention), and to follow workers for any decline in lung function that may occur from dust/fume exposure (secondary prevention). However, there is no consensus on how often to screen potentially affected workers, as different exposures create different risks.8 The “norm” seems to be yearly testing, but that may not be sufficient in high risk areas.8 In summary, spirometry screening in individual patients (eg, a smoker being treated for hypertension and who has no pulmonary symptoms) is no longer an “official” recommendation.9 That same patient, however, if employed in a high risk industry, may well have spirometry testing once a year. OSHA has published guidelines for spirometry screening in various industries.10 It is currently mandatory for workers exposed to various substances, including asbestos, cadmium, coke ovens, cotton dust, benzene, formaldehyde, methylene chloride, and silica dust.11 —Lawrence Martin, MD |
References
- Miller MR, Crapo R, Hankinson J, et al. General considerations for lung function testing. Eur Respir J. 2005;26:153-61.
- Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26:219-328.
- Hyatt R, Scanlon P, Nakamura M. Interpretation of Pulmonary Function Tests. A Practical Guide. 3rd ed. Philadelphia: Wolters Kluwer Lippincott Williams & Wilkins; 2009.
- Enright P. Does screening for COPD by primary care physicians have the potential to cause more harm than good? Chest. 2006;129:833-5.
- The Use of Spirometry for Case Finding, Diagnosis, and Management of Chronic Obstructive Pulmonary Disease (COPD). Agency for Healthcare Research and Quality. Available at: www.ahrq.gov/clinic/tp/spirotp.htm. Accessed May 1, 2010.
- Pruitt B. Spirometry screening for COPD? Maybe not? RT for Decision Makers in Respiratory Care. 2009;22(2):26, 28, 29.
- Lin K, Watkins B, Johnson T, et al; US Preventive Services Task Force. Screening for chronic obstructive pulmonary disease using spirometry: summary of the evidence for the US Preventive Services Task Force. Ann Intern Med. 2008;148:535-43.
- Harber P, Levine J, Bansal S. How frequently should workplace spirometry screening be performed? Chest. 2009;136:1086-94.
- Screening for chronic obstructive pulmonary disease. US Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;148:529-34.
- United States Department of Labor Occupational Safety & Health Administration. Available at: www.osha.gov (search spirometry). Accessed May 1, 2010.
- BarnesCare. Pulmonary Function Test (Spirometry) FAQs. Available at: http://www.barnescare.com/barnescare07_content.aspx?id=4448. Accessed May 1, 2010.