Nitric oxide (NO) is a ubiquitous molecule in the human body and essential to regulatory mechanisms of multiple organ systems. In its endothelial cell derived form, NO plays a central role in regulating vascular tone. Endogenously produced NO activates guanyl cyclase in endothelial cells, leading to increased production of cyclic guanasine monophosphate (cGMP). The increase in cGMP levels results in an efflux of calcium from cells, and relaxation of the endothelial smooth muscle cell. In its inhaled form (iNO), NO readily diffuses from the alveolar space to the pulmonary vascular smooth muscle cell and acts as a selective pulmonary vasodilator. Once crossing into the pulmonary circulation, iNO is quickly inactivated by binding with hemoglobin in the erythrocytes, so there is no systemic vasodilatory effect when iNO is administered. iNO is preferentially delivered to well-ventilated areas of the lung, hence redistributing pulmonary blood flow and helping to lessen ventilation-perfusion mismatch, with resultant improvement in oxygenation.
Randomized trials of iNO in late preterm and term infants with hypoxic respiratory failure and/or persistent pulmonary hypertension of the newborn (PPHN) demonstrated improved oxygenation and a reduction in the use of extracorporeal membrane oxygenation (ECMO) with its administration.1,2 It is FDA-approved for use in this population, and it has become a mainstay in the management of PPHN; its use has, in part, been responsible for the reduction in the use of ECMO nationally.
The role of iNO therapy in premature infants with respiratory failure remains unclear and controversial. Despite improved survival of extremely low birth weight infants with surfactant therapy and antenatal glucocorticoids, bronchopulmonary dysplasia (BPD, defined as an oxygen requirement at 36 weeks postmenstrual age) remains an important and frequent adverse outcome.3 In both laboratory studies and animal models of BPD, iNO has additional and potentially beneficial effects on the developing lung beyond the reduction in pulmonary arterial pressure. These include reduction in inflammation and oxidant stress; bronchodilatation and decreased airway smooth muscle proliferation; and improvement in angiogenesis, lung growth, and surfactant function.4-7 The preclinical studies have heightened interest in iNO as a potential therapy for treatment of respiratory failure in preterm infants and as a preventive therapy to avoid the development of BPD. In this review, I will outline the rationale for the use of iNO in premature infants and summarize the results of recent randomized, controlled clinical trials.
Animal Models of BPD: Effects of iNO
Animal models of BPD provide insight into the potential benefits of iNO in preterm infants. Current evidence suggests that the pathology of BPD includes an arrest of lung development, with impaired alveolarization and simplification of the lung architecture.3 Similar changes in lung development are observed in mice genetically deficient in endogenous nitric oxide production, and its exogenous replacement can result in improved alveolarization and lung growth,8-10 suggesting an important role of NO in early lung development. iNO therapy in early life may also prevent some of the pathological changes seen in evolving BPD. For example, in a lamb model, low dose iNO started after birth during a 3-week course of mechanical ventilation resulted in decreased airway resistance and smooth muscle proliferation, and improved alveolarization.11 In a baboon model, exposure to iNO during mechanical ventilation for 14 days improved lung mechanics as well as lung growth as measured by total lung weight, DNA, and total protein content.7
Lung inflammation caused by exposure to high inspired oxygen content and mechanical ventilation also plays a critical role in the pathogenesis of BPD. Neutrophil influx into the lung is an early marker of the acute lung injury associated with the development of BPD in preterm infants,12 and it may be modulated by use of iNO. In a preterm lamb model of respiratory distress syndrome, low dose iNO improved gas exchange and decreased neutrophil accumulation in the lung.5 In addition, iNO may protect the preterm lung against oxidant stress. In one study, preterm lambs ventilated with iNO showed no evidence of lung oxidative stress injury compared to those ventilated without iNO.6 Similar results have been observed in other animal models combining exposure to a hyperoxic environment and iNO.13,14 The results of the animal models suggest that more prolonged exposure to iNO might be necessary to see benefits in decreased lung injury and improved lung repair in the preterm population, in contrast to the usually briefer duration of exposure for treatment of persistent pulmonary hypertension in term infants.
Human Trials
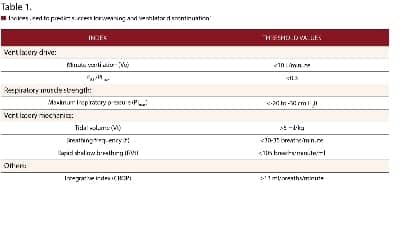
There have been multiple human trials investigating the effects of iNO in preterm infants. These trials are heterogeneous and differ in study design, enrollment criteria, and the dose and duration of iNO use, making comparisons difficult. Clinical outcomes reported include acute effects on oxygenation, death, the incidence of survival without BPD, intraventricular hemorrhage (IVH), and periventricular leukomalacia (PVL), as well as long-term neurodevelopmental outcomes. The Cochrane Collaboration has performed a review of the use of iNO for respiratory failure in preterm infants,15 but, because of significant differences in study design, a true meta-analysis of randomized trials is not possible. In this review, studies were divided into three categories depending on entry criteria: 1) rescue treatment (initiation of iNO in the first 3 days based on oxygenation criteria); 2) routine “prophylactic” use for intubated, mechanically ventilated infants; and 3) delayed enrollment based on increased risk for BPD. The largest randomized, controlled trials to date of iNO therapy in preterm infants include the single center study of Schreiber et al16 and the multicenter trials of Van Meurs et al,17 Kinsella et al,18 and Ballard et al,19 each of which will be reviewed in detail below. Major outcomes are summarized in Tables 1 and 2.
 |
 |
Rescue Treatment
Van Meurs et al enrolled 420 infants (401 to 1,500 gram birth weight) in a randomized controlled trial performed in the National Institutes of Health Neonatal Research Network.17 This study was designed to assess the acute effects on oxygenation of 5 to 10 ppm of iNO in preterm infants with hypoxic respiratory failure, with the major outcome measure being the incidence of survival without BPD. Despite a study design that included enrollment of infants with moderate respiratory disease (oxygenation index [OI] of 10, later modified to 5), it also included infants who had severe lung disease, with the mean OI at study entry of 23 for the group randomized to iNO and 22 for placebo. Enrolled infants were approximately 24 hours old, with a mean birth weight of 840 grams, and gestational age of 26 weeks. The study design mandated discontinuation of study gas if there was no acute response to initiation (defined as an increase in PaO2 of at least 20 mm Hg), so that the average duration of iNO exposure was only 57 hours. Overall, the study found no differences in the incidence of BPD or death between the infants who received iNO compared to placebo (80% and 82%, respectively; P = 0.52). However, in a post hoc analysis of the infants who weighed less than 1,000 grams at enrollment (n = 158), both mortality and the incidence of severe IVH/PVL were significantly higher in the infants who received iNO. Although the incidence of death or BPD was decreased for infants with a birth weight greater than 1,000 grams, the small number of enrolled infants in this birth weight category (n = 52) casts some doubt on the significance of this finding.
Routine “Prophylactic” Treatment
Two major trials have reported results of routine iNO use in preterm infants requiring mechanical ventilation in the first days after birth. Schreiber et al, in a single-center trial, randomized 207 infants to treatment with iNO (10 ppm for 24 hours, then 5 ppm for 6 days or until extubated) or placebo.16 Enrolled infants were larger (mean birth weight of approximately 1,000 grams), a week older in gestational age (27 weeks), and significantly less ill (average OI 6.94) than those enrolled in the Van Meurs trial. The main finding was a reduction in the incidence of BPD or death by 24% in the iNO group (48.6% versus 63.7%; P = 0.03). These benefits appeared to be limited to infants with less severe lung disease; the decrease in death or BPD was observed only in infants with an OI on study entry less than the average of 6.94.
Another intriguing and unexpected outcome of this trial was a 47% decrease in the incidence of severe IVH or PVL in the iNO treated infants (12.4% versus 23.5%; P = 0.04). Moreover, follow-up of the infants at 2 years of age also showed overall improved neurodevelopmental outcomes in the infants randomized to iNO, suggesting that iNO, as used in this trial, may be neuroprotective for a subset of preterm infants.20 Other complications of prematurity were unchanged with iNO therapy.
In the largest published trial to date of routine use of iNO, Kinsella et al randomized 793 premature infants with birth weights between 500 and 1,250 grams, who required mechanical ventilation in the first 48 hours, to iNO (5 ppm for 21 days or until extubated) or placebo.18 Enrolled infants had a mean birth weight of 790 grams and gestational age of 25.5 weeks, with an average OI on enrollment of 5.4, and duration of iNO exposure of 14 days. The main finding of this study was no significant difference in the incidence of BPD or death in the iNO compared to placebo groups (71.6% versus 75.3%, respectively; P = 0.24). However, in a preplanned subgroup analysis, iNO decreased the incidence of BPD or death in the infants with a birth weight of more than 1,000 grams. Similar to the Schreiber study, Kinsella also found that iNO was neuroprotective with a significant decrease in the combined outcomes of severe IVH, PVL, and ventriculomegaly in the entire study group (17.5% versus 23.9%; P = 0.03). Despite the differences in early neurological complications associated with iNO, no differences in the incidence of neurodevelopmental impairment were observed by treatment assignment among survivors at 1 year of age.21
These two studies suggest that iNO is safe, and its early use may have a role in pulmonary protection for a subpopulation of preterm infants with a birth weight greater than 1,000 grams and milder lung disease who require mechanical ventilation beyond 48 hours of age. The mechanisms by which iNO may offer neuroprotection are unclear and require further study.
Late Treatment of Infants at Risk for BPD
In a study design markedly different from the randomized trials described above, Ballard et al conducted a study in which 582 infants with a birth weight between 500 and 1,250 grams were randomized to receive iNO (20 ppm for 72 hours, decreased weekly for a total duration of therapy of 24 days) or placebo if they continued to require mechanical ventilatory support between 7 and 21 days of age, a group at high risk to develop BPD.19 Enrolled infants had an average birth weight and gestational age of approximately 760 grams and 26 weeks, with an estimated OI of about 7. In this study, the incidence of BPD or death was significantly decreased in the infants given iNO (56.1% versus 63.2%, respectively; P = 0.04); this benefit was almost entirely derived from the subset of infants who were enrolled at 7 to 14 days, however. Of note, the results also suggested less severe BPD in treated infants, with a higher percentage of iNO treated infants being discharged home by 40 and 44 weeks postmenstrual age. Improvements in pulmonary outcomes persisted into childhood, with less bronchodilator use in iNO treated infants at 1 year of age.22 A recent economic analysis also suggested that despite its associated costs, iNO as used in the Ballard trial was cost-effective due to the decrease in BPD and reduction in overall hospital length of stay.23
Summary and Recommendations
Although iNO is a safe and effective therapy in the treatment of late preterm and term newborns with pulmonary hypertension and respiratory failure, its role in the premature infant has been more difficult to define. In contrast to its use in term infants, for the preterm infant, effects of iNO other than pulmonary vasodilatation, including modulation of inflammation, oxidative stress, and lung growth, are likely more important. As indicated by the clinical trials to date, the effects of iNO in the preterm infant may be dependent on the timing, dose, and duration of therapy, as well as on the nature and severity of their lung disease.
Currently, given the available data, it seems prudent to avoid the use of iNO in extremely low birth weight infants who have severe hypoxic respiratory failure, since it may worsen outcome. As a preventive therapy, a 24-day course of iNO when used in preterm infants less than 1,250 grams birth weight, who continue to require mechanical ventilation at 7 to 14 days of age following the Ballard protocol, appears to be safe, helps reduce the risk of developing BPD, and improves pulmonary outcomes. Use of this treatment strategy is a reasonable approach while awaiting additional clinical data.
Eric C. Eichenwald, MD, is associate professor of pediatrics, Baylor College of Medicine, Texas Children’s Hospital, Houston.
References
- Clark RH, Kueser TJ, Walker MW, et al. Randomized, controlled trial of low-dose inhaled nitric oxide treatment of persistent pulmonary hypertension of the newborn. Clinical Inhaled Nitric Oxide Group. N Engl J Med. 2000;17:342:469-74.
- Inhaled nitric oxide in full-term and nearly full-term infants with hypoxic respiratory failure. Neonatal Inhaled Nitric Oxide Study Group. N Engl J Med. 1997;336:597-604.
- Eichenwald EC, Stark AR. Management and outcomes of very low birth weight. N Engl J Med. 2008;358:1700-11.
- Kinsella JP, Ivy DD, Abman SH. Inhaled nitric oxide improves gas exchange and lowers pulmonary vascular resistance in severe experimental hyaline membrane disease. Pediatr Res. 1994;36:402-8.
- Kinsella JP, Parker TA, Galan H, Sheridan BC, Halbower AC, Abman SH. Effects of inhaled nitric oxide on pulmonary edema and lung neutrophil accumulation in severe experimental hyaline membrane disease. Pediatr Res. 1997;41:457-63.
- Storme L, Zerimech F, Riou Y, et al. Inhaled nitric oxide neither alters oxidative stress parameters nor includes lung inflammation in premature lambs with moderate hyaline membrane disease. Biol Neonate. 1998;73:172-81.
- McCurnin DC, Pierce RA, Chang LY, et al. Inhaled NO improves early pulmonary function and modifies lung growth and elastin deposition in a baboon model of neonatal chronic lung disease. Am J Physiol Lung Cell Mol Physiol. 2005;288:450-9.
- Han RN, Babaei S, Robb M, et al. Defective lung vascular development and fatal respiratory distress in eNOS deficient mice: a model of alveolar capillary dysplasia? Circ Res. 2004;94:1115-23.
- Balasubramaniam V, Tang JR, Maxey A, Plopper CG, Abman SH. Mild hypoxia impairs alveolarization in the endothelial nitric oxide synthase-deficient mouse. Am J Physiol Lung Cell Mol Physiol. 2003;284:L964-71.
- Tang JR, Markham NE, Lin YJ, et al. Inhaled nitric oxide attenuates pulmonary hypertension and improves lung growth in infant rats after neonatal treatment with a VEGF receptor inhibitor. Am J Physiol Lung Cell Mol Physiol. 2004;287:L344-51.
- Bland RD, Albertine KH, Carlton DP, MacRitchie AJ. Inhaled nitric oxide effects on lung structure and function in chronically ventilated preterm lambs. Am J Respir Crit Care Med. 2005;172:899-906.
- Ogden BE, Murphy S, Saunders GC, Johnson JD. Lung lavage of newborns with respiratory distress syndrome. Prolonged neutrophil influx is associated with bronchopulmonary dysplasia. Chest. 1983;83(5 suppl):31S-33S.
- Nelin LD, Welty SE, Morriset JF, Gotuaco C, Dawson CA. Nitric oxide increases the survival of rats with a high oxygen exposure. Pediatr Res. 1998;43:727-32.
- Issa A, Lappalainen U, Kleinman M, Bry K, Hallman M. Inhaled nitric oxide decreases hyperoxia-induced surfactant abnormality in preterm rabbits. Pediatr Res. 1999;45:247-54.
- Barrington KJ, Finer NN. Inhaled nitric oxide for respiratory failure in preterm infants. Cochrane Database Syst Rev. 2007;(3):CD000509.
- Schreiber MD, Gin-Mestan K, Marks JD, Huo D, Lee G, Srisuparp P. Inhaled nitric oxide in premature infants with the respiratory distress syndrome. N Engl J Med. 2003;349:2099-107.
- Van Meurs KP, Wright LL, Ehrenkranz RA, et al. Inhaled nitric oxide for premature infants with severe respiratory failure. N Engl J Med. 2005;353:13-22.
- Kinsella JP, Cutter GR, Walsh WF, et al. Early inhaled nitric oxide therapy in premature newborns with respiratory failure. N Engl J Med. 2006;355:354-64.
- Ballard RA, Truog WE, Cnaan A, et al. Inhaled nitric oxide in preterm infants undergoing mechanical ventilation. N Engl J Med. 2006;355:343-53.
- Mestan KK, Marks JD, Hecox K, Huo D, Schreiber MD. Neurodevelopmental outcomes of premature infants treated with inhaled nitric oxide. N Engl J Med. 2005;353:23-32.
- Watson RS, Clermont G, Kinsella JP, et al. Clinical and economic effects of iNO on premature newborns with respiratory failure at 1 year. Pediatrics. 2009;124:1333-43.
- Hibbs AM, Walsh MC, Martin RJ, et al. One-year respiratory outcomes of preterm infants enrolled in the Nitric Oxide (to prevent) Chronic Lung Disease trial. J Pediatr. 2008;153:176-82.
- Zupancic JA, Hibbs AM, Palermo L, et al. NO CLD Trial Group. Economic evaluation of inhaled nitric oxide in preterm infants undergoing mechanical ventilation. Pediatrics. 2009;124:1325-32.