Anticipating and Overcoming Airway Difficulties
Obesity can exacerbate OSA and presents special intubation problems. RTs need to be prepared with strategies when treating this patient population
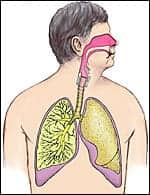
 Obesity is reaching epidemic proportions in the United States.1 According to the National Center for Health Statistics,2 approximately 30% of adults aged 20 years or older are obese, with obesity defined as a body mass index (BMI) or kg/m2of 30 or more. Airway access in obese patients is an ongoing concern for clinicians and respiratory care personnel. It has long been recognized that obesity makes intubation and extubation difficult.3,4 Planning ahead and anticipating airway management difficulties related to obesity are cornerstones of management.
Obesity is reaching epidemic proportions in the United States.1 According to the National Center for Health Statistics,2 approximately 30% of adults aged 20 years or older are obese, with obesity defined as a body mass index (BMI) or kg/m2of 30 or more. Airway access in obese patients is an ongoing concern for clinicians and respiratory care personnel. It has long been recognized that obesity makes intubation and extubation difficult.3,4 Planning ahead and anticipating airway management difficulties related to obesity are cornerstones of management.
Sleep Apnea Studies
Much of our understanding of airway management in obese patients comes from studies of patients with sleep apnea.5,6 A substantial proportion of the adult population has mild-to-moderate sleep apnea, a condition characterized by repeated episodes of apnea and hypopnea during sleep. According to the American Lung Association,7 as many as 18 million Americans suffer from sleep apnea.
The reduction of tonic upper airway dilating muscle activity caused by sleep is associated with reduced upper airway caliber and increased pharyngeal wall compliance.8 The mechanical corollary of decreased caliber is an increase in upper airway resistance.9 In addition to increased resistance, increased pharyngeal wall compliance during sleep in snorers is manifested by the occurrence of inspiratory flow limitation as flow plateaus during inspiration.9
The combination of increased resistance and inspiratory flow limitation leads to an increased work of breathing, hypoventilation, and frequent arousals from sleep, and ensuing excessive daytime sleepiness. This has been described as a distinct clinical entity referred to as the upper airway resistance syndrome.10
The association between obesity and sleep apnea is well recognized. Weight gain in patients with sleep apnea usually results in an increase in the severity of apnea. It has long been hypothesized, and later documented by magnetic resonance imaging (MRI), that the region surrounding the collapsible segment of the pharynx in patients with sleep apnea has a greater fat load than does the same region in equally obese patients who do not have sleep apnea. This finding—in conjunction with the finding of an increase in airway resistance and a decrease in airway stability documented when applying lard-filled bags to the neck to simulate cervical fat accumulation—suggests that the effect of obesity on sleep apnea might be related to local parapharyngeal fat deposits.11 Histopathologic studies of uvulas excised during uvulopalatopharyngoplasty for sleep apnea have demonstrated higher amounts of both fat and muscle mass compared with those seen during normal postmortem studies.12,13
 Much of our understanding of airway management in obese patients comes from studies of patients with sleep apnea
Much of our understanding of airway management in obese patients comes from studies of patients with sleep apnea
Management Considerations
Obese patients may require multiple intubation attempts and the use of accessory airway devices, according to the results of a large-scale retrospective analysis14 involving 1,253 consecutive emergency intubations (not including those performed in the operating room) over a 12-year period. Of the 1,253 patients, 174 (13.9%) were morbidly obese (with a BMI of more than 40). In the study sample, 72% of patients with a BMI of less than 25 could be intubated on the first attempt, compared with only 52% of those who were morbidly obese. Among the morbidly obese patients, 18% required three attempts for successful intubation, compared with only 10.5% of the normal-weight patients. Similarly, accessory airway devices were required by many more morbidly obese patients than normal-weight patients (58% versus 22%). Bougies were required by morbidly obese patients 21% of the time, compared with 10% of the time in normal-weight patients. Laryngeal mask airways were required by 28% of the morbidly obese patients, compared with only 4% of the normal-weight patients. Kritensen and Mort14 also noted that many obese patients required the use of a special ramp and blankets to optimize head and neck position for intubation. These observations underscore the need to recognize that obese patients may require more intensive airway management than normal-weight patients. Investigators have studied the effectiveness of the laryngeal airway mask in morbidly obese patients undergoing bariatric surgery. In one prospective, observational study performed by Frappier et al,15 the rate of successful tracheal intubation in morbidly obese patients was 96.3%.
Conclusions
Airway management in the obese patient can be challenging, as airway difficulties are often complicated by obesity. Respiratory care personnel should consider strategies to anticipate and manage patients with difficult airways. This includes identifying the potential problem, considering different options, and selecting an appropriate plan for the individual patient.
In morbidly obese patients, normal anatomic landmarks may be obscured. Tracheal intubation and extubation decisions in morbidly obese persons should be made with the consideration that there may be excess pharyngeal tissue that cannot be visualized by routine examination.
John D. Zoidis, MD, is a contributing writer for RT.
References
1. Centers for Disease Control and Prevention. Overweight and Obesity: Frequently Asked Questions (FAQs). 2006. Available at: www.cdc.gov/nccdphp/dnpa/obesity/faq.htm Accessed August 10, 2006.
2. National Center for Health Statistics. Prevalence of Obesity Among Adults: United States, 1999-2002. 2004. Available at: www.cdc.gov/nchs/products/pubs/pubd/hestats/obese/obse99.htm Accessed August 10, 2006.
3. Rocke DA, Murray WB, Rout CC, Gouws E. Relative risk analysis of factors associated with difficult intubation in obstetric anesthesia. Anesthesiology. 1992;77:67-73.
4.Rose DK, Cohen MM. The airway: problems and predictions in 18,500 patients. Can J Anaesth. 1994;41:372-83.
5. Netzer NC, Hoegel JJ, Loube D, et al. Prevalence of symptoms and risk of sleep apnea in primary care. Chest. 2003;124:1406-14.
6. Bixler EO, Vgontzas AN, Ten Have T, Tyson K, Kales A. Effects of age on sleep apnea in men: I. Prevalence and severity. Am J Respir Crit Care Med. 1998;157:144-8.
7. American Lung Association. Sleep Apnea (Sleep-Disordered Breathing). Available at: www.lungusa.org/site/pp.asp?c=dvLUK9O0E&b=34706&ct=357715 Accessed August 23, 2006.
8. Tangel DJ, Mezzanotte WS, White DP. Influence of sleep on tensor palatini EMG and upper airway resistance in normal men. J Appl Physiol. 1991;70:2574-81.
9. Shepard JW, Pevernagie DA, Stanson AW, Daniels BD, Sheedy PF. Effects of changes in central venous pressure on upper airway size in patients with obstructive sleep apnea. Am J Respir Crit Care Med. 1996;153:250-254.
10. Guilleminault C, Stoohs R, Clerk M, Cetel M, Maistros P. A cause of excessive daytime sleepiness: the upper airway resistance syndrome. Chest. 1993;104:781-7.
11. Suratt PM, McTier RF, Wilhoit SC. Collapsibility of the nasopharyngeal airway in obstructive sleep apnea. Am Rev Respir Dis. 1985;132:967-71.
12. Sher AE. An overview of sleep disordered breathing for the otolaryngologist. Ear Nose Throat J. 1999;78:694-5, 698-700, 703-6.
13. Walker RP, Grigg-Damberger MM, Gopalsami C, Totten MC. Laser-assisted uvulopalatoplasty for snoring and obstructive sleep apnea: results in 170 patients. Laryngoscope. 1995;105:938-43,
14. Kristensen E, Mort TC. Morbid obesity: risky airway business. Presented at: Society of Critical Care Medicine 35th Critical Care Congress. January 7-11, 2006; San Francisco. Abstract 109-M.
15. Frappier J, Guenoun T, Journois D, et al. Airway management using the intubating laryngeal mask airway for the morbidly obese patient. Anesth Analg. 2003;96:1510-15.